- What Is the Gut Microbiome?
- What You Will Learn
- Impact of Gut Dysbiosis on Your Health
- What Factors Contribute to Dysbiosis?
- How to Support Your Gut
- Good Bacteria vs. Bad Bacteria
- The Gut-Brain Axis
- Bacterial Strains and Their Implications in Health and Disease
- How Can You Modulate Your Gut Microbiome?
- Frequently Asked Questions (FAQ)
- Conclusion
Did you know that most of the cells in your body aren’t human? Your body consists of about 37 trillion cells. In comparison, there are around 100 trillion microbes living in and on your body, creating a complex ecosystem called a microbiota that holds the key to your health and well-being.
What’s more, approximately 70% of your microbiota is in your gut. As a result, there’s a direct connection between the bacteria that live in your gut, your lifestyle, and your risk of developing chronic diseases!
In other words, lifestyle factors such as diet and exercise can change the makeup of your gut’s microbiome. Understanding the relationship between these variables and the bacterial composition of your intestines can help support overall gut health, cure a leaky gut, and reduce your risk of developing a chronic disease like cancer, heart disease or diabetes.
What Is the Gut Microbiome?
The human gut microbiome, also known as the gut flora or gastrointestinal microbiota, is an intricate and intertwined community of microorganisms (such as bacteria) that live in your digestive tract. No two humans have the exact same microbiome.
Your well-being depends on the health of your unique gut microbiome.
The microbiome begins to form in the womb, and continues developing during infancy and throughout our lives. Each species of bacteria that lives in our body has its own unique genetic structure, and each interacts with our body in different ways. Some assist with digestion and immune response; others make vitamins, help us utilize minerals, or help us process substances like protein, fat and fiber.
Scientists first observed microbes under a microscope in the 17th century. More than 200 years later, scientists discovered that so-called opportunistic microbes are the cause of diseases like cholera and tuberculosis. For many years, we thought that because microbes were the cause of diseases, we should eradicate them.
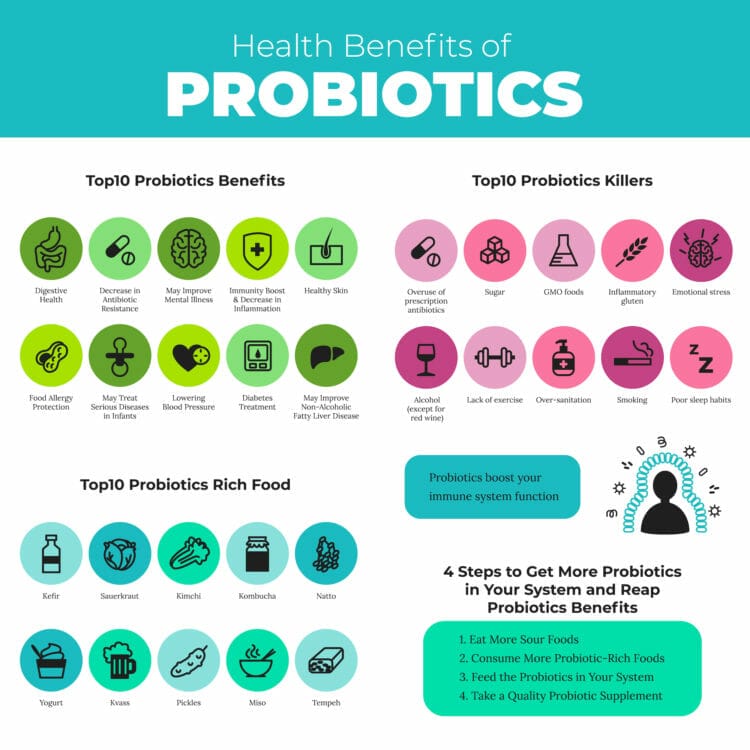
Later, scientists realized that there are also “good bacteria,” also known as probiotics, and that sweeping them all off from the mucous membranes of our bodies would do more harm than good.
In other words, bacteria can be beneficial. Modern science has proven that certain microbial strains fight off diseases and their symptoms.
In terms of gut health, that means your body has to maintain a balance between good and bad bacteria.
Here are some interesting facts and figures about your gut microbiota:
- It’s home to about 3.3 million genes, as compared to the approximately 23,000 human genes.
- It’s composed of bacteria, archaeabacteria (which are similar to bacteria), viruses, and yeast-like single-cell eukaryotes.
- You can find 400 to 1,500 different species in a healthy digestive tract.
- There are around 35,000 microbial species across all of mankind.
- 99% of your gut microbes are from 30 to 40 species.
- Diversity is the number one defining feature of a healthy microbiome.
What You Will Learn
In this article, you’ll learn why balancing the microbes that colonize your body is crucial for your health. We’ll review how the gut microbiome strongly influences the brain, the blood, and even our emotions. And we’ll look at how we can modulate (influence) these bacteria to our advantage.
I’ll also show you an easy way to test your gut flora at home to learn more about your intestinal microbiome composition. I did two of these tests and was fascinated by the results — and especially by the microbial diversity (which indicates how many different types of microbes live in my gut).
Benefits of a Healthy Gut Microbiota
As we discussed above, the microorganisms in your gut play a key role in maintaining health and well-being. Here are some of the benefits provided by your gut microbiota.
- Digestion (carbohydrate, protein and fat metabolism)
- Vitamin synthesis
- Phytochemical absorption
- Production of neuroactive compounds
- Regulation of gut barrier integrity (to prevent leaky gut)
- Immune system regulation
Digestion
Without our gut microbiota we wouldn’t be able to digest and metabolize fiber, starches and sugars (carbohydrates), protein or fat.
Our bodies only have 17 so-called carbohydrate-active enzymes (CAZymes). The remaining 10,000+ come from the bacteria in our gut, such as Bacteroides, and they’re important for digesting carbs. The main byproducts of that carb metabolism are short-chain fatty acids — including acetate, propionate and butyrate — that play vital roles in reducing inflammation, blood-sugar control, fat metabolism and more.
In order for our bodies to use protein, it has to be broken down into amino acids. While gastric enzymes such as protease help with that process, most of the microbes in our gut are also proteolytically active. That means they can break down protein into amino acids and even create them from scratch!
Did you know that 20 to 30% of the carbs and 10% of the protein we consume doesn’t get digested by gastric enzymes? It’s the microbes in our gut that take care of that.
Gut bacteria also regulates fat metabolism in the small intestines, which is home to far fewer microbes than the large intestine.
Vitamin Synthesis
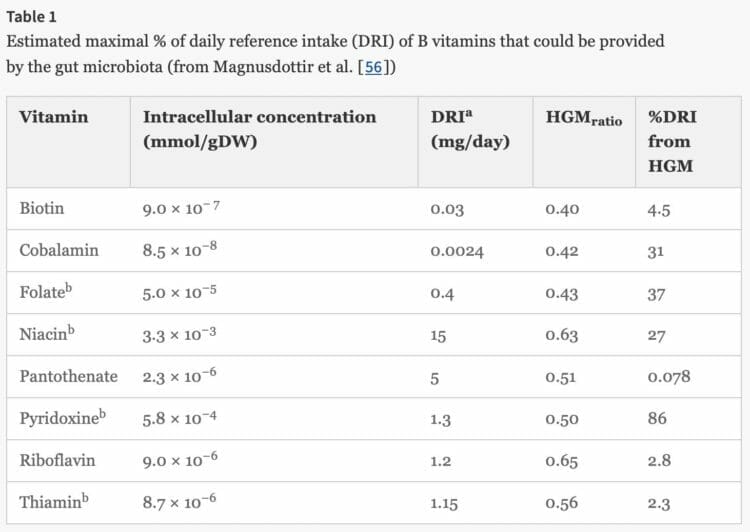
While there is a concern that we might not get the nutrients we need entirely from the food we eat, you should know that the bacteria in our gut can make vitamins!
Fun fact: Vitamin B12 is the most complex vitamin to make. It takes 60 chemical reactions to synthesize it!
For example, our microbiota makes a significant number of the B vitamins, via a process called vitamin synthesis. Among other things, B vitamins are vital for converting nutrients into energy, producing DNA, red blood cells or protecting cells by acting as antioxidants.
Have you heard about Vitamin K2? Chances are, you haven’t but scientists believe it could be the missing link between food and certain diseases. Specifically, studies have shown that Vitamin K2 increases the calcification of bones and decreases the calcification of blood vessels and the kidneys. More calcium in bones leads to stronger bones and less calcium in blood vessels decreases your risk of developing heart disease.
The interesting part is that we can’t get Vitamin K2 directly from food. The bacteria in our gut makes it by sourcing building blocks from certain food we eat, including meat, pasture raised eggs and fermented food.
Phytochemical Absorption
Phytochemicals are micronutrients and biologically-active compounds found in plants. So far, scientists have identified over 10,000 phytochemicals (such as polyphenols) but only a few have been studied in detail. As a result, we don’t fully understand yet how those compounds can influence the chemical processes in our bodies.
Some plant-based advocates believe phytochemicals play an important role in our overall health and well-being. According to the American Institute for Cancer Research, phytochechemicals have the potential to:
- Stimulate the immune system
- Block substances we eat, drink and breathe from becoming carcinogens
- Reduce the kind of inflammation that makes cancer growth more likely
- Prevent DNA damage and help with DNA repair
- Reduce the kind of oxidative damage to cells that can spark cancer
- Slow the growth rate of cancer cells
- Trigger damaged cells to commit suicide before they can reproduce
- Help to regulate hormones
While I appreciate the potential of phytochemicals for medicinal use cases, I have not seen any credible paleoanthropological or scientific evidence that humans need those compounds to enjoy optimal health.
Be aware that not all phytochemicals are beneficial to our health. For example, phytic acid (inositol) is a phytochemical and an antinutrient that can inhibit the absorption of minerals. On the other hand, beta-carotene, a carotenoid, works as an antioxidant and you can find it in broccoli, carrots, leafy greens and other veggies. Unfortunately, all those plants are also loaded with defense chemicals that negate any benefits you might get from beta-carotene.
Unfortunately, our body can only absorb around 5% of the identified 10,000 phytochemicals directly. The remaining 95% are broken down and metabolized by the bacteria in our gut. As a result, phytochemicals can influence the composition of our gut microbiota by acting as a prebiotic (food for probiotics). Whether or not that has a net-positive effect on our health, I’m not convinced of.
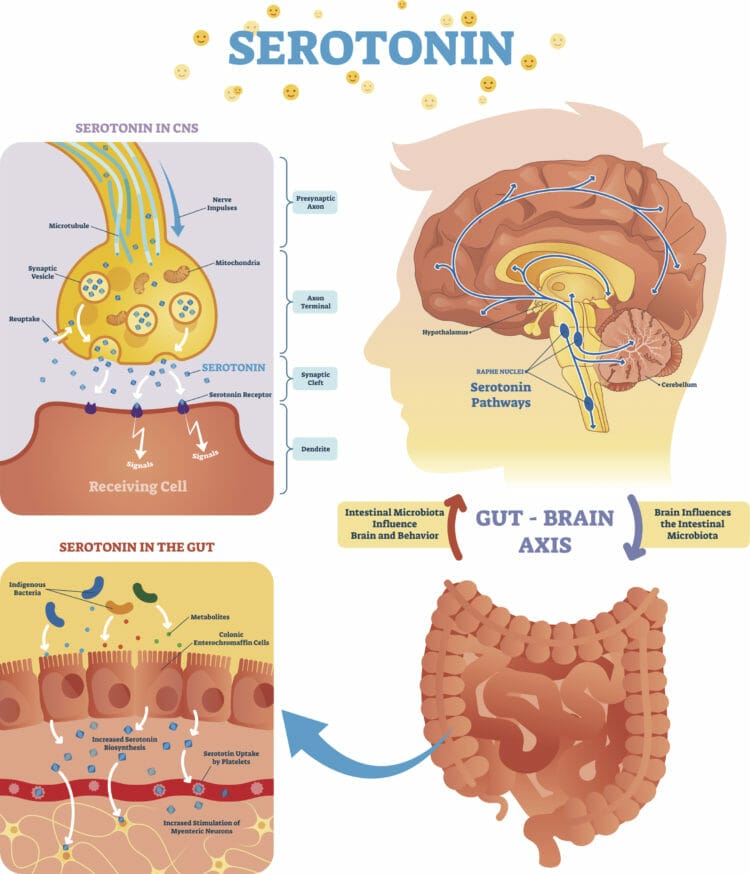
Production of Neuroactive Compounds
Our gut microbiome also has a direct impact on our brain through the production of neurotransmitters, which are chemical substances that regulate the communication between nerve fibers. Think of nerve fibers (axons) as the communication highway in our brain. The more such connections we have, the better our brain works.
Additionally, the microorganisms in our gut also regulate the blood-brain barrier, which controls the transfer of nutrients and other chemical compounds to our brain via the bloodstream.
Regulation of Gut Barrier Integrity
If the tight junctions of the interior lining of your gut are permeable, then the contents of your gut, including toxins, can flow unregulated into your bloodstream, causing inflammation and chronic diseases. That condition is called leaky gut or permeability of the gut.
The good bacteria in your gut regulates the gut barrier integrity, thus reducing the chance of inflammation.
Immune System Regulation
They say that every disease starts in your gut. And that’s true, because the majority of your immune system is located in your gut. In other words, the microbes in your gut modulate the production and activation of T and T helper (Th) cells, which are responsible for your body’s immune response.
Impact of Gut Dysbiosis on Your Health
A gut dysbiosis is an imbalance of your gut microbiota, and it can lead to or interfere with the treatment of numerous health-related issues.
- Inflammatory bowel disease (IBD): High levels of certain opportunistic bacteria strains can trigger the development and symptoms of Crohn’s disease and ulcerative colitis.
- Irritable bowel syndrome (IBS): There is a strong connection between IBS and an overgrowth of bacteria in the small intestines (SIBO). (On a side note, here’s how I cured my own IBS.)
- Mood disorders: The lack of certain probiotics has been linked to depression and anxiety.
- Schizophrenia: Studies in mice and prematurely-born infants have shown a connection between a low biodiversity and higher risks of schizophrenia.
- Cardiovascular (heart) disease: Certain bacteria that thrive on grains have been shown to convert the amino acid L-carnitine (found in red meat) into a compound called TMOA, which increases the risk of developing heart disease. That might be one of the reasons why some studies have suggested that red meat is bad for your health.
- Cancer: A dysbiosis has been linked to various forms of cancers and carcinomas affecting the liver, colon, stomach, gallbladder, pancreas and breast.
- Obesity and diabetes: Gut microbes directly influence the metabolism and the associated signaling pathways which affect inflammation, how fat is stored, insulin resistance and more.
- Obsessive-compulsive disorder (OCD): There is a correlation between a dysfunction of the gut microbiome — potentially related to stress or the use of antibiotics — and OCD.
- Autism: Patients diagnosed with autism often also suffer from GI issues, such as leaky gut and IBS. Recent studies have demonstrated the long-term benefit of microbiota transfer therapy on autism symptoms and gut microbiota.
- Neurological disorders (Alzheimer’s and Parkinson’s disease): Many neurological disorders start with insulin resistance and lead to an impaired glucose metabolism of the brain, such as in the case of Alzheimer’s. Observational studies have shown that people suffering from neurological disorders usually have a different microbial composition than healthy individuals.
- Multiple sclerosis (MS): Scientists have linked MS to dysbiosis and an imbalance in the gastrointestinal immune response.
- Asthma and allergies: A low microbial diversity in the gut, especially early in life, is linked to an increased risk of asthma and allergies.
- Rheumatoid arthritis: Studies have found that people with low numbers of good bacteria (probiotics) and high numbers of opportunistic bacteria have a higher risk of developing autoimmune issues, such as rheumatoid arthritis.
In a nutshell, if your microbiota is out of balance you significantly increase your chances of developing a chronic or metabolic disease.
What Factors Contribute to Dysbiosis?
Below is a list of factors that can contribute to dysbiosis. Remember, if your microbial diversity is out of balance — meaning you have too many harmful or opportunistic and not enough beneficial and commensal bacteria — you significantly increase your risk of developing a chronic disease.
- Nutrient deficiencies: Make sure you eat a healthy diet and, if necessary, use supplements.
- Dehydration: Make sure to drink enough water, tea or black coffee, and stay away from sugar-laden beverages.
- Prolamins and agglutinins: These harmful and inflammatory proteins are found in grains such as wheat, rye, barley, oats and corn.
- Alcohol: Consume alcohol in moderation (or use a high-quality alcohol alternative).
- Non-nutritive sweeteners: One more reason to stay away from artificial sweeteners.
- Excess sugar and refined starches: No surprise here, and maybe a good reason to start looking into a low-carb ketogenic diet.
- High omega-6 polyunsaturated fat intake: That’s one of the reasons why your proportion of omega-3 to omega-6 is so important, and why you should stay away from most vegetable oils.
- Digestive enzyme inhibitors: Certain grains, such as wheat, can significantly lower the amounts of digestive enzymes. Yet another reason to avoid grains in your diet.
- Emulsifiers, preservatives and additives: Try to stay away from processed foods, and eat fresh, organic and raw food instead.
- Casein and soy protein: Casein, a protein found in most dairy and soy, can negatively impact the tight junctions in your gut (thus causing a leaky gut).
- Stress: Make sure to manage your stress and try to reduce it through exercise, meditation and sleep.
- Inactivity and overtraining: Neither inactivity nor overtraining are beneficial for your gut, so find the right balance and exercise at moderate intensity as often as you can. For CrossFitters like me, holding back is not always easy but it’s necessary.
- Inadequate sleep: Protect your sleep by any means possible, even if it’s socially awkward. Being constantly sleep deprived is not a sign of strength but stupidity.
If you don’t make sure to avoid the factors I mentioned above, your gut becomes permeable, systematic inflammation sets in, you become insulin resistant, and you ultimately develop a chronic disease.
How to Support Your Gut
Did you know that 60% of the composition of your microbiota is determined by diet? The remaining 40% is determined by lifestyle and exposure to environmental factors, such as toxins, genetics, age and hormones.
Supporting your gut follows the same three principles as maintaining a healthy lifestyle in general:
- Eat healthily
- Exercise regularly
- Get enough sleep
Both exercise and quality sleep relieve stress, which is a mechanism that can impact the composition and function of the bacteria in your intestines.
Maintain a Healthy Diet

The food you eat directly influences the array of microbes in your gut. Every type of bacteria thrives on certain kinds of food for fuel. Some like carbs, while others prefer fat, protein or fermented foods.
If you want to reduce the number of a particular type of microbe in your gut, starve them of the foods they like.
On the flip side, if you want your good bacteria to thrive and keep harmful bacteria at bay, you need to maintain a healthy dietary lifestyle. Eating a diet rich in sugars, processed carbs, grains and dairy will lead to a dysbiosis (a microbial imbalance or maladaptation), and ultimately to the development of chronic diseases.
In other words, a diet that feeds all the “wrong” bacteria while not providing enough food for the “good” ones may have significant negative long-term health implications.
Fun fact: According to an analysis of my gut microbiota, I have less gluten-digesting microbes than people who report no ailments and a high level of wellness. While I don’t have celiac disease (as far as I know), my relatively low number of those bacteria is likely because I avoid grains in my diet. That deprives them of the fuel they need to expand their colony.
Best Foods to Support a Healthy Gut Microbiome
Below is a high-level overview of the best foods you can eat and other factors to support a healthy gut:
- Micronutrients: Eat organic whole foods that are rich in micronutrients, such as vitamins and minerals.
- Protein: Look for pastured and wild-caught fish, chicken, pork and beef and stay away from soy and pasteurized dairy (especially casein).
- Amino acids: Some of the building blocks of proteins have been shown to be extra beneficial for the gut, including arginine and glutamine.
- Fats: The microbes in your gut prefer Omega-3s over monounsaturated and saturated fats.
Stay tuned for an in-depth article discussing the best foods to support a healthy gut!
Exercise Regularly

Based on scientific studies, regular exercise can increase the microflora diversity in your gut. The proliferation of bacteria can then modulate mucosal immunity and improve barrier functions, thus reducing the risk of obesity and metabolic diseases.
The mucosal immune system determines how well your body can protect itself against pathogens and environmental toxins. The better that immune system works, and the better it blocks such pathogens from getting into your bloodstream (barrier function), the less likely you get sick and develop systematic inflammation — the root cause of metabolic ailments.
Get Enough Sleep
The gut-brain axis connects the gut and the brain (see below). And you probably already know that the brain is responsible for managing sleep, via the release of certain hormones (such as melatonin) via the pineal gland.
However, the body has a backup plan for many critical functions, including the release of melatonin. If the pineal gland isn’t functioning adequately, the gut can jump in and assist by converting the amino acid tryptophan into serotonin.
The body can then further convert serotonin into melatonin, a sleep hormone that manages the body’s circadian rhythm. It’s another example of how your “second brain” (the gut) can influence chemical processes that are entirely unrelated to digestion.
Good Bacteria vs. Bad Bacteria

We are hosts to billions or even trillions of bacterial cells, most of which are located on the external and internal linings of the body. Microbes populate our skin and the mucosa of the gastrointestinal tract, the urinary tract, and many other surfaces of our body. Many of those microorganisms are so-called “commensal microbes,” which do not have any effect on our health (that we know of today).
Others are beneficial bacteria (probiotics) that provide extra nutrients, increase our body’s defenses, and modulate specific metabolic processes. Both beneficial bacteria and commensal microbes compete against harmful pathogens. They colonize the surface of the skin and mucosa, eliminating that space that virulent microbes would use to take root and subsequently cause disease.
In other words, the healthy bacteria on our skin and in our gut fill up the “empty space” and prevent harmful bacteria from colonizing and causing problems.
If you're healthy, there is no "empty" space in your gut that's not already populated by bacteria. That's why supplementing with probiotics might not work if the bacterial strains in the supplement don't have room to settle in. Adding bacteria to your gut's microbiome is all about displacing and replacing what's already there. That makes modulating the microbiota in your gut a long-term process that often requires changes in your lifestyle.
Moreover, recent scientific initiatives, such as the International Human Microbiome Consortium and the Human Microbiome Project, have been studying how specific changes in the balance of good bacteria have an impact on our health and the development of chronic diseases.
However, similarly to healthy bacteria, pathogens can colonize the gut and fill the available space. When that happens, healthy bacteria will find it difficult to set in — even if we try to add them through probiotics.
That’s why taking a prebiotic or probiotic supplement often “enhances” your gut flora only temporarily — or for as long as you take the supplement.
The Gut-Brain Axis
During its evolutionary formation, the gut was optimized as a means to absorb nutrients. However, it needed an integration center, as well as sensory and executive pathways that allowed our bodies to expel toxins and unwanted contents (and to fight off pathologic bacteria). The neuronal connection in the gut was essential for that process to work correctly, and it became an independent network from that of the brain.
This “gut brain” contains around 200 million neurons. That’s incredible, considering that the brain functions properly with “only” 86 billion neurons. In time, the human body integrated the two neuronal systems and started to share several functions that complement each other.
Even though the connection between the brain and the gut was evident for many years, recent studies have revealed a very complex system of interaction between the gastrointestinal tract and brain function. It appears that the microbiota is capable of modulating the function of the brain by releasing neurotransmitters, chemical messengers, hormones, and even metabolites (as in the case of short-chain fatty acids).
For example, Bifidobacterium species in the human gut produce a neurotransmitter called gamma-aminobutyric acid (GABA), which is an inhibitory neurotransmitter that may have an analgesic effect and may even reduce abdominal pain from a neuronal perspective.
Another example is Lactobacillus rhamnosus, which is a common probiotic strain to control post-antibiotic diarrhea. These bacteria cause a change in the expression of GABA receptors in the brain and reduce psychiatric symptoms such as anxiety and depression.
On the other hand, pathogen species such as Streptococcus, Enterococcus, Escherichia, and Candida produce a neurotransmitter called serotonin, which scientists have linked to anxiety, depression, impulsive behavior and other mental health problems. Similarly, there are many other examples of how gut microbiota is capable of changing essential aspects of our health, such as the modulation of pain, changes in mood and certain mental diseases.
The gut is not only linked to the central nervous system, however. It is also profoundly related to the immune system through an extensive network of lymphoid tissue that’s associated with the mucosa of the gastrointestinal tract. This is why recent studies report that certain bacterial strains have a positive effect on autoimmune diseases such as inflammatory bowel disease (chronic inflammation), rheumatoid arthritis, asthma and others.
Bacterial Strains and Their Implications in Health and Disease
After putting all the evidence together, scientists have realized that the gut is more than just a digestive organ. It’s a valuable player for maintaining and promoting health, and can even contribute to the prevention of several chronic diseases. We now understand that the genes of our gut microbiota and their molecular activity directly influence the expression of genes in the rest of our body.
Thus, there is a great deal of current research about several bacterial strains which are beneficial for our health. These are just a few of the most important:
- Lactobacillus acidophilus
- Lactobacillus rhamnosus
- Lactobacillus reuteri
- Bifidobacterium species
Lactobacillus Acidophilus
Lactobacillus acidophilus is one of the members of a group called lactic acid bacteria. They are usually found in fermented foods like sauerkraut, tempeh, miso and yogurt.
This bacterial strain has been found to modulate the immune system and reduce the severity of several vaginal disorders such as vaginosis and candidiasis (yeast infection). It is capable of fighting off Helicobacter pylori and reduces the incidence of several other infections in the gastrointestinal system.
Lactobacillus acidophilus is also used to prevent allergic disorders such as allergic rhinitis and dermatitis. Additionally, it reduces antibiotic-induced diarrhea and may be helpful for treating inflammatory bowel disease and other bowel problems.
No wonder so many different brands use Lactobacillus acidophilus as an additive in yogurt and similar products. It’s also a common ingredient in probiotic supplements, often being combined with other strains like bifidobacteria and Streptococcus salivarius. There are many subtypes of lactobacilli within the acidophilus group, and we don’t yet fully understand the mechanisms by which they promote health.

Lactobacillus Rhamnosus
Lactobacillus rhamnosus is a bacterial strain that was discovered when scientists began their search for another lactobacillus strain that could survive stomach acid. They wanted to find a suitable candidate for a probiotic supplement. Lactobacillus rhamnosus has the structure of a rod, and it produces a compound called bacteriocin, which has potent antimicrobial activity against Pseudomonas, Escherichia coli, Salmonella, Staphylococcus, Streptococcus and other pathogens.
Thus, this bacterial strain is often used to prevent the colonization of pathogens, to kill them off, and to revert antibiotic-induced diarrhea.
An interesting finding is that people who receive Lactobacillus rhamnosus strains along with antibiotics would also benefit from the health effects of these bacteria. Studies report that this bacteria retains the ability to colonize the human gut during antibiotic treatment.
These bacteria adhere firmly to the epithelium of the intestine, which makes it even harder for other pathogens to colonize. Lactobacillus rhamnosus helps prevent and treat infectious diarrhea, reduces the incidence of allergic diseases in children, and has been used for atopic eczema treatments. Finally, this strain has a potential anti-obesity effect because it modulates obesity biomarkers such as fatty acid synthase.
Lactobacillus Reuteri
Lactobacillus reuteri is also known as strain F275 to avoid confusion with Lactobacillus fermentum in the scientific literature. One of the most critical properties of Lactobacillus reuteri is the synthesis of a molecule called reuterin, and another called reutericyclin. These molecules are capable of killing pathogen bacteria, protozoa and fungi.
Additionally, L. reuteri produces several vitamins, including folic acid, vitamin B12 and thiamine, making them available for absorption into the bloodstream. Similarly to many other bacterial strains in the gut microbiota, L. reuteri is capable of regulating immune function by suppressing proinflammatory cytokines and causing a local reduction of allergies in the gastrointestinal tract.
According to various studies, L. reuteri administration in infants reduces the crying time caused by infant colics. It’s helpful in necrotizing enterocolitis and in preventing several infectious and inflammatory diseases in the colon.
Bifidobacterium Species
There are many Bifidobacterium species, and the most important in the field of probiotics are bifidobacterium animalis spp lactis, Bifidobacterium bifidum, Bifidobacterium breve, and Bifidobacterium longum. In the case of B. animalis spp lactis, it survives the acidity of the stomach without a problem, has been shown to accelerate the bowel movements in people suffering from constipation, and reduces minor gastrointestinal symptoms such as bloating and distention in healthy patients.
This strain has anti-inflammatory properties and may reduce the severity of several inflammatory diseases, primarily when they are located in the gastrointestinal tract.
Bifidobacterium bifidum is another significant strain under these probiotic species. It reduces the incidence of eczema, is useful in managing radiation-related diarrhea and rotavirus-induced diarrhea, reduces the risk of infection of Clostridium difficile, and has been found to be beneficial for immune function in elderly patients.
On the other hand, Bifidobacterium longum exerts potential anti-inflammatory effects which are helpful in preventing diseases such as ulcerative colitis and may help normalize bowel function in elderly patients.
The studies on Bifidobacterium breve are usually focused on the immunomodulatory role in infants and children for preventing food allergies, atopic dermatitis, asthma and other immune-related diseases.
How Can You Modulate Your Gut Microbiome?
As we have reviewed in this article, the gut is one of the largest organs in the body. It’s linked to the central nervous system, immune function, and modulates several molecules and metabolic processes. However, improving the gut’s microbiome might be more complicated than you think.
It’s not only about buying and taking expensive probiotic supplements. We also need to reduce harmful bacteria to make room, and carefully choose bacterial strains with antibacterial activity to replace them.
That’s why I recommend making naturally prebiotic and probiotic food part of your diet. For example, you can eat sauerkraut several times a week as a side dish.
Supplements can certainly help if you’re making the transition from an unhealthy to a healthy diet, or if you’re on antibiotics due to an infection or other diseases. However, don’t think you can get away with using supplements while maintaining a lifestyle that’s not conducive to healthy gut flora.
Frequently Asked Questions (FAQ)
The Microbiome Diet is a new diet that touts a restoration of gut health and claims to aid in weight loss.
Frankly, if you have a healthy dietary lifestyle — one that is characterized by eating fresh food that mimics what our ancestors ate for millions of years — you don’t need to do anything extra to support your gut.
The food our ancestors ate was covered in bacteria, but much of our food today is highly-processed and refined, resulting in products that are unnecessarily “clean.” So if you’re not following Paleolithic eating habits, you may want to consider the use of high-quality prebiotic and probiotic supplements to compensate.
One of my favorites is Terraflora’s Synbiotic formula, which is a broad spectrum, soil-based blend that contains strains proven to resist biological stressors such as heat and stomach acid.
The stomach and proximal small intestine contain relatively few microorganisms, mostly because of the presence of gastric acid, which makes those parts of your gastrointestinal tract an unpleasant home for bacteria.
However, there is a medical condition known as small intestinal bacterial overgrowth (SIBO) or small bowel bacterial overgrowth (SBBO), which is defined as an increase in the number of bacteria in the upper GI tract.
There are a number of different ways to evaluate the makeup of your microbiome, but the easiest by far is using the at-home test offered by uBiome. All you have to do is request a testing kit, place a couple of small stool samples in the provided plastic containers, and mail them back to uBiome in the pre-paid (sanitary) packaging. uBiome leverages the latest DNA sequencing technology and research from the NIH Human Microbiome Project to give you unprecedented access to all the information that lies in your gut microbiome. I recently took this test and found it absolutely fascinating.
Update: uBiome filed for bankruptcy in 2019 and stopped all operations.
As a Crossfit enthusiast, I knew about the vital role of BCAAs in muscle synthesis and recovery. However, research on piglets has shown that BCAAs are also involved in maintaining an intestinal barrier function. A study conducted by Japanese researchers has demonstrated “that dietary supplementation with BCAAs promotes intestinal development, enhances enterocyte proliferation, increases intestinal absorption of amino acids (AA) and glucose, and improves the immune defenses.”
Leaky gut (also known as intestinal permeability) is a condition in which the cells in the intestinal linings become permeable, thus allowing toxic nutrients into your bloodstream.
Research has shown that eating a diet high in grains, legumes and other foods containing antinutrients increases the risk of developing leaky gut. Research also suggests that maintaining a healthy gut microbiome can help counter the effects of these antinutrients.
Insulin sensitivity (diabetes) is a metabolic disease that is often caused by systematic inflammation. In the same way that your diet influences the microbiome in your gut, you can modulate those inflammatory pathways through the diet you eat.
An altered gut microbiome may contribute to obesity, which in turn can promote insulin resistance.
Bile acids are organic compounds in bile that facilitate the digestion and absorption of lipids (fatty acids) in the small intestine.
Eating a diet that’s high in healthy fats can undoubtedly change the composition of your microbiota. Additionally, eating unhealthy fats, such as vegetable oils that are high in omega-6 fatty acids, can negatively impact your gut and your overall health by causing inflammation and intestinal permeability.
If you decide to follow a high-fat diet, such as the ketogenic diet, it’s particularly important to pay attention to the health of your microbiome because recent research has shown that gut bacteria play a key role in the absorption and metabolism of dietary fat, allowing you to get “get more calories for the same foods,” according to the Carnegie Institution for Science.
Some smart marketers claim that taking probiotic supplements can prevent or treat diseases like schizophrenia, autism and many others.
Scientific evidence strongly suggests that most chronic ailments, including mental diseases, are influenced or caused by lifestyle choices and diet in particular. However, it would be a mistake to think that taking a probiotic supplement can outweigh an otherwise crappy diet. That’s not how it works.
However, supplements are proven to help with conditions such as antibiotic-induced diarrhea and travelers’ diarrhea, and in some cases have been shown to help with ulcerative colitis, food allergies and vitamin deficiencies.
If you choose to use a supplement, I recommend a high-quality brand, such as Terraflora or Performance Lab.
The bacteria in your gut eat both fiber and protein, and require two important amino acids (glutamine and arginine) to thrive. Without these two key substances, your diversity of gut bacteria can shrink.
Conversely, making sure you have the right amount of amino acids can help correct a dysbiosis, making supplements a viable option.
Interestingly, some bacteria participate in a process called bacterial crossfeeding, in which they eat the metabolites (poop) of other bacterial species. What this means is that gut biodiversity is subject to the network effect — if your microbiome is healthy today, it will become even healthier over time.
Phytochemicals are biologically-active compounds produced by plants. In fact, they’re primarily what give the foods we eat their color. For example, phytochemicals are what make strawberries red and blueberries blue. However, these compounds also have an array of health benefits, including a reduction in the risk of major chronic diseases. That’s largely because many of them act as antioxidants.
Currently, there are about 5,000 known phytochemicals. The precise biological impact of most of them remains unclear, as only a few dozen have been studied in detail. Scientists also believe there are thousands more as-yet-unidentified phytochemicals.
Only about 5% of known phytochemicals are absorbed directly. The rest are broken down, processed and metabolized in our gut by bacteria.
I recently learned that the polyphenols (naturally-occurring plant compounds) in tea can have a positive impact on your gut. There’s emerging evidence that tea polyphenols can improve your gut microbiome by supporting the growth of probiotic strains like Lactobacillus and suppressing the growth of pathogenic bacteria like C. difficile.
One of my favorite tea products is Pique Tea Crystals, which have 12x the antioxidants of regular tea. If you like tea and are looking for a way to support your gut health, I recommend giving them a try.
Conclusion
Besides increasing our consumption of fermented foods and probiotic supplements, there are a few other things we can do on a day-to-day basis to positively modulate our gut microbiota.
Reducing stress, sleeping properly, maintaining a diet with sufficient fiber, and engaging in moderate exercise may improve our overall health and promote the growth of healthy gut bacteria. These measures will not only modulate our microbiome but also contribute to our general health and improve our quality of life.

Michael is a healthy living enthusiast and CrossFit athlete whose goal is to help people achieve optimal health by bridging the gap between ancestral living and the demands of modern society.
Medical Disclaimer
The information shared on this blog is for educational purposes only, is not a substitute for the advice of medical doctors or registered dieticians (which we are not) and should not be used to prevent, diagnose, or treat any condition. Consult with a physician before starting a fitness regimen, adding supplements to your diet, or making other changes that may affect your medications, treatment plan or overall health. MichaelKummer.com and its owner MK Media Group, LLC are not liable for how you use and implement the information shared here, which is based on the opinions of the authors formed after engaging in personal use and research. We recommend products, services, or programs and are sometimes compensated for doing so as affiliates. Please read our Terms and Conditions for further information, including our privacy policy.