- What Is Irritable Bowel Syndrome (IBS)?
- My Experience With IBS From Childhood to Adulthood
- How I Cured Irritable Bowel Syndrome (Almost Overnight)
- My Search for an IBS Cure Continued
- How I Permanently Cured IBS
- 6 Steps You Can Take Cure Your IBS Symptoms
- Frequently Asked Questions
- Wrap-Up: When It Comes to IBS, Managing the Symptoms Doesn’t Fix the Problem
Irritable bowel syndrome (IBS) is a catch-all term for gastrointestinal symptoms, including abdominal pain, bloating, cramping, constipation, diarrhea and erratic bowel movements. IBS can last for months or even years, thus dramatically reducing the quality of life for those affected.
My dad has suffered from IBS since he was a kid. I did as well, until I finally figured out what was causing it.
In this article, I’ll share my experience with chronic gut issues and explain the simple lifestyle change I introduced that made my IBS symptoms disappear within a few days.
What Is Irritable Bowel Syndrome (IBS)?
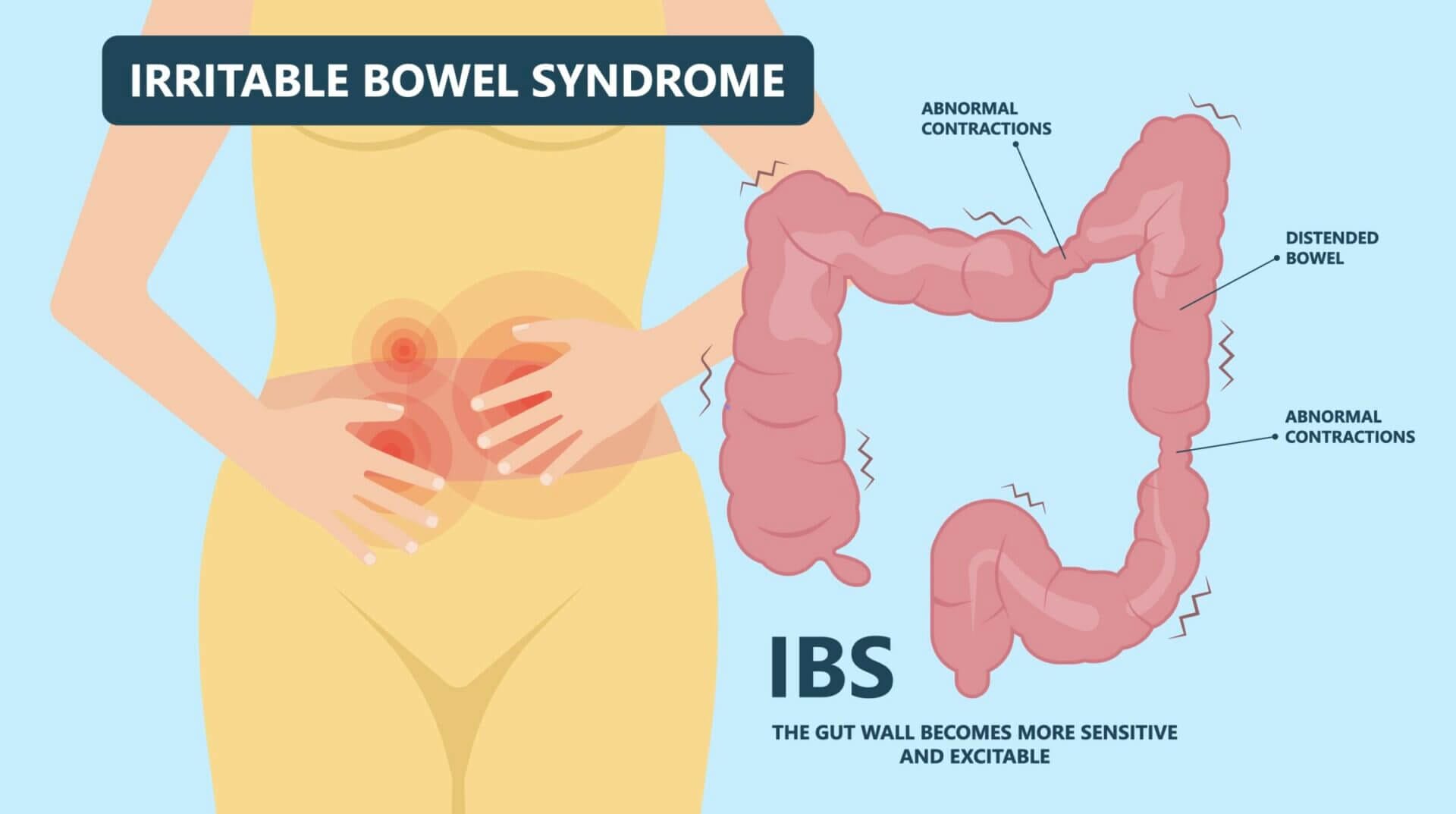
According to the Mayo Clinic, “irritable bowel syndrome (IBS) is a common disorder that affects the large intestine. Signs and symptoms of IBS include cramping, abdominal pain, bloating, gas, and diarrhea or constipation, or both. IBS is a chronic condition that you’ll need to manage long term.”
Depending on the individual symptoms, IBS can be divided into several subtypes, including IBS-C, IBS-D and IBS-M.
The truth is that IBS is a phrase that describes symptoms that aren’t caused by any of the other known inflammatory bowel diseases (IBD), such as colitis, Crohn’s disease and ulcers.
In other words, if your healthcare provider can’t determine what’s causing your issues, they’ll call it IBS. At least, that’s what happened in my case.
My Experience With IBS From Childhood to Adulthood

When I was a kid, my dad was always eating something different than the rest of the family. He claimed he was sensitive to many of the foods we grew up with in Austria, like dairy, veggies, legumes and most grains.
One day, he even flipped over a casserole my mom made for him because it had onions in it — one of the veggies that triggered his symptoms. I don’t know for sure, but I believe my mom felt like he was making up most of his symptoms and thus snuck onions into his meal because she figured he wouldn’t notice (and she firmly believed every meal tasted better with onions).
I also remember my dad telling my brother and me that it was just a matter of time until we’d experience similar GI issues, because our grandpa also suffered from similar ailments all his life, up until he died of stomach cancer in his late 40s.
Little did he know that both my brother and I had already experienced the onset of IBS at that time, but the symptoms weren’t severe enough to raise any red flags.
Specifically, I was often bloated and/or constipated, leading to longer-than-normal potty breaks. As I grew older, my symptoms got worse. I recall one day during a youth summer camp where my belly was so bloated that I couldn’t even walk upright without suffering agonizing pain.
As time passed, I began to accept that GI issues were a regular part of my life. During my 20s and most of my 30s, it didn’t even occur to me that none of the symptoms I was experiencing were normal.
But most of the time, I could manage them if I just had a toilet nearby that I could use — or if I was able to pass gas without bothering anyone.

When I met my wife in 2009, I learned that she also had chronic gut issues, manifesting in frequent bloating, heartburn, abdominal pain and diarrhea.
How I Cured Irritable Bowel Syndrome (Almost Overnight)
Up until 2013, my wife and I both followed a standard American diet that was rich in grains, processed carbohydrates and vegetable oils. But after watching the documentary Fat, Sick and Nearly Dead on Netflix, about the health implications of consuming massive amounts of added sugars, we started implementing dietary changes, beginning with avoiding sugar-laden foods.
That documentary sparked my curiosity about the impact food has on our health. In 2015, a friend inspired me to go on a paleo diet that was supposed to mimic what early humans and our Paleolithic ancestors would have eaten (but using modern foods).
As part of that dietary transition, we removed entire food categories from our plates, including:
- Artificial sweeteners.
- Cereal grains.
- Legumes (peanuts, beans, lentils, tofu).
- Processed foods.
- Refined sugar.
- Refined vegetable oils.
- Soda and other sweetened beverages.
At the beginning of our paleo journey, most of our meals consisted of a piece of beef, chicken or fish, paired with grilled vegetables, such as peppers, carrots or zucchini.
Within a few days, all my gut issues had disappeared and I felt great for the first time in decades. No more bloating and discomfort after meals! I could finally feel comfortable leaving the house without strategically planning my bathroom breaks. I felt liberated!
For the next couple of months, I experienced no IBS symptoms. And I figured I was cured.
But a few months into our paleo journey, we began embracing a more society-friendly version of this diet that included baked goods made with nut flours and starches made from tubers, to name a few of the “paleo upgrades” we made.
We even purchased several cookbooks that taught us how to make everyday dishes paleo-friendly.
The unintentional side effect of that transition was that we significantly increased the variety of foods we ate. We also ate more of specific food categories, including nuts and seeds, than in the past.
After a few weeks on this “modern” paleo diet, my IBS symptoms returned in full force. I was shocked and couldn’t explain it, because I thought the paleo diet had cured my IBS permanently.
My Search for an IBS Cure Continued
So I went to my primary care physician, who referred me to a gastroenterologist to perform a gastroscopy. This procedure involved swallowing a tube with a camera attached to the front, enabling the doctor to look for signs of inflammation, bleeding or ulcers.
Fortunately, the gastroscopy didn’t reveal any damage to my stomach or the upper part of my small intestine (which is as far as the tube reaches).
Next, my doctor tested me for small intestinal bacterial overgrowth (SIBO) that he thought could be causing the bloating I was experiencing after meals. However, the SIBO test came back negative too.
Considering that my doctor couldn’t diagnose the problem, he told me I had what’s known as irritable bowel syndrome (IBS). He also said that many of his patients had the same issue, and that there was no cure.
He didn’t think it would make a huge difference, but suggested trying to implement dietary changes, such as avoiding FODMAPs.
If you’re reading this, you’ve probably heard about FODMAP. It stands for fermentable oligosaccharides, disaccharides, monosaccharides and polyols, which are short-chain carbohydrates (sugars) that the small intestine absorbs poorly. Foods high in FODMAPs include dairy, cereal grains, legumes, nuts and many fruits high in fructose.
I wasn’t convinced that pursuing a low-FODMAP diet would help, because I firmly believed that paleo was the healthiest diet there was. Plus, I didn’t want to cut out many of the “healthy foods” I regularly ate, including nuts, seeds and vegetables.
Instead, I was sure I had some sort of bacterial overgrowth and I continued to pursue additional tests, including one for helicobacter pylori and antibodies in my blood that could indicate food sensitivities. I also had my stools analyzed to check for parasites and an abundance of certain opportunistic bacteria, such as E. coli, clostridium and others.
Unfortunately, none of those tests were conclusive. Some even turned out to be inherently unreliable, such as the IgG-based food sensitivity tests. So I was back at square one.
The Keto Diet Made My Symptoms Worse

As I learned more about the impact of food on human metabolism and how our ancestors ate for millennia, I decided that our paleo diet was no longer good enough.
I was convinced that a very low-carb (ketogenic) diet would improve our health and cure my gut issues.
As you might know, keto is an elimination diet that doesn’t allow the consumption of most sweet fruits and starchy veggies.
But much like with the modern paleo diet, there are different approaches to following a ketogenic diet. For example, we learned various ways to make regular dishes (especially treats and baked foods) keto-friendly by leveraging nut butter, nut flours, non-caloric sweeteners and low-carb veggies, including cauliflower, garlic and onions.
Unfortunately, the foods I ate as part of my low-carb journey worsened my IBS, and I grew increasingly frustrated.
How I Permanently Cured IBS


At some point during my search for a cure, I remembered the reason why I embarked on a Paleolithic diet in the first place: to mimic the diet that allowed our ancestors to thrive and evolve into modern humans.
Then it occurred to me that what I was eating every day bore little resemblance to the diet of our ancestors.
In other words, I was consuming massive amounts of processed foods that our ancestors either didn’t have access to (such as nut butter and seed oil) or that they only consumed during certain times of the year (such as fruits and veggies).
So I decided to implement a fairly dramatic change by removing all foods that could potentially upset my digestive system.
Based on my research, I learned that all plants (to varying degrees) have compounds, including FODMAPs and defense chemicals, that can wreak havoc on the digestive system. So the first step was to cut out all plants, dairy and eggs from my diet.
All I was left to eat was meat and seafood.
Within a few days, my IBS symptoms disappeared and I felt great again.
Next, I began reintroducing certain foods, including pasture raised eggs, sweet fruits and some veggies, to see what would trigger my symptoms.
Some triggers I discovered included inulin (a prebiotic fiber found in artichokes, bananas, onions, wheat and other plants), garlic, nuts and nut flours, sweet potatoes, leafy greens and others.
The discovery that plant-based foods were the root cause of my gut issues ultimately led me to an animal-based diet consisting mainly of protein and fat from muscle meat and organs, raw honey, seasonal sweet fruits, raw dairy and some of the least-toxic plants (e.g., cucumbers, zucchini and squash).
These days, the entire Kummer household follows an animal-based diet that takes into account what each of our individual bodies can tolerate.
For example, our youngest son Lucas doesn’t do well with eggs. At the same time, our oldest daughter appears to have a relatively robust digestive system that can even handle the occasional nut-flour-based muffin.
Fortunately, we’ve learned through trial and error which foods trigger our symptoms, so we don’t have to be on a strict carnivore diet. Instead, we can include some seasonal sweet fruits, the least-toxic veggies and raw honey.
Aside from Lucas, we also enjoy fresh eggs from our hens, and dairy (including raw milk).
6 Steps You Can Take Cure Your IBS Symptoms
If you’ve been suffering from IBS or similar digestive issues, including Crohn’s disease, colitis or ulcers, I highly recommend taking the following steps:
- Remove all plant foods from your diet immediately.
- Cut out eggs and dairy. The lactose and casein in the latter can worsen your symptoms.
- Avoid alcohol (or use a high-quality alcohol alternative).
- Consume only meat, organs and raw honey for 30-90 days.
- Consider using supplements that can help heal your gut (see below).
- Once your symptoms have subsided, slowly reintroduce the least-toxic plant foods.
As I discussed in my article comparing meat vs. plants, all plants have defense chemicals (antinutrients such as lectins and oxalates) that deter animals and humans from eating them. In comparison, animals fight or run away to deter you from eating them.
By removing the toxins found in plant foods from your diet, you allow your gut to heal. While I consider raw dairy a healthy source of nutrients, some people can’t tolerate it, so I recommend avoiding dairy products at first. You can reintroduce them later once your gut has healed. Alcohol is another toxin that has the potential to irritate the delicate lining inside your gut, so cut it out for a few weeks.
The good news is that you can eat as much meat as you like. Still, I recommend sticking with the meat and organs from ruminants (e.g., cows, goats, sheep and venison) and limiting your intake of meat from monogastric animals (like pork and chicken) because it’s naturally higher in linoleic acid, an inflammatory polyunsaturated fatty acid (PUFA). You can also enjoy wild-caught seafood.
Of course, when I say “meat,” I mean fresh, unprocessed and unseasoned meat. Consuming marinated meat or adding spices will likely irritate your gut and prevent it from healing. The only seasoning you can and should use liberally is salt (ideally a high-quality Himalayan or comparable salt).
Note: Wondering what the science says about my recommendation? Researchers at Harvard University studied over 2,000 people on a carnivore diet and found that 97% “improved or resolved gastrointestinal conditions” after they stopped consuming most plat-based foods.
As far as supplements to assist in your gut-healing journey are concerned, you can consider:
- Bovine colostrum. The insulin-like growth factors in bovine colostrum can help stimulate the regeneration and proliferation of cells in the gut lining (epithelium). Check out my article about the health benefits of bovine colostrum and my list of top colostrum supplements to learn more.
- Ancient dirt water. We buy a liquid mineral supplement called ION Gut Health made from ancient dirt water to help strengthen the cellular barriers in our gut and other body parts. (Use code MICHAELKUMMER to get 15% off.)
- Ozone oil. Ozone has a number of health benefits, and ozone oil can help treat parasites in the gut and other inflammatory issues. We use a product from SimplyO3.
- Spore-based probiotics. Spore-based or soil-based probiotics can help reestablish a healthy gut microbiome. My favorite product in this category is Terraflora from Enviromedica.
- Digestive enzymes. This can help with breaking down the extra fat and protein you’ll be consuming while your pancreas adjusts by increasing its enzyme production. I like MassZymes from biOptimizers.
- Magnesium. Magnesium is an important mineral that helps your gut move food along as it gets digested. BiOptimizers Magnesium Breakthrough is the magnesium supplement we use every day before bedtime.
Once you’re free of symptoms, you can slowly start reintroducing raw dairy, sweet fruits, avocados, olives and the least-toxic plants, including de-seeded and peeled squash, zucchini and cucumbers.
From there, I highly recommend sticking with a predominantly animal-based diet for the rest of your life. Doing so dramatically increases your chances of maintaining a healthy gut and avoiding most of the chronic diseases that Americans suffer from.
Non-Pharmaceutical Methods to Relieve the Symptoms of Irritable Bowel Syndrome
While you implement the tips I outlined above, there are a couple of methods that can help improve your symptoms that don’t require prescription medication, including:
- Physical activity. I always felt better during and after light physical activity, because being active can help with gut motility.
- Relaxation techniques. Sauna bathing, breathing exercises and meditation are great ways to relax and change how you perceive the symptoms of IBS.
One thing I’ve learned over the past few years is that stress can have a major impact on my health and well-being. By learning to control how you respond to stress by down-regulating the sympathetic branch of your nervous system, you can positively influence your gut health.
To learn more check out my article about how I manage stress and the benefits of ice baths and cold water immersion.
Frequently Asked Questions
It’s possible, but unlikely. While there are several lifestyle factors that can cause IBS (or influence its progression), diet is usually the main culprit. Once your digestive system has started malfunctioning, it’s almost impossible for it to get back to a normal state if you don’t address the root cause of the issue.
That’s why I recommend making substantial dietary changes to allow your gut to heal and your IBS symptoms to subside. Once your gut is working optimally again, it’s OK to reintroduce some of the foods you enjoyed before (because that chances are a healthy digestive system can handle them).
There are four types of subcategories of IBS that are defined by the symptoms patients experience, including IBS-D (mostly diarrhea and abdominal discomfort), IBS-C (mostly constipation and abdominal discomfort), IBS-mixed (alternating loose stools and constipation with abdominal discomfort) and the undefined subtype IBS-U, which presents with various symptoms.
The good news is that the methods presented in this article are applicable to all four IBS types. In other words, lifestyle and dietary factors are at the root cause at all four types and so the cure is the same. Looking back at the mixed symptoms I suffered from for three decades, I suppose I was in the IBS-mixed camp.
While certain plants have a place in a species-appropriate diet, most plants contain defense chemicals that can negatively impact the health of the digestive system. Plants don’t want to be eaten, so they’ve developed chemical weapons (called antinutrients) to deter people from consuming them. You can learn more in my article comparing meat vs. plants.
Yes, gluten is an inflammatory protein that can trigger IBS symptoms. That’s why I recommend removing cereal grains and other processed foods that might be contaminated with gluten from your diet.
Studies have shown that cognitive behavioral therapy (CBT) can be an effective tool for treating the symptoms of IBS and other gastrointestinal disorders, because of the connection between the gut and brain via the nervous system (aka gut-brain axis).
However, I consider CBT a complementary treatment option to dietary changes. If you keep adding fuel to the fire by consuming inflammatory foods, you won’t be able to succeed in the long-term treatment of IBS.
Removing all carbohydrates from your diet (meat doesn’t have any carbs) increases your body’s electrolyte demands, so it’s important to increase your electrolyte intake (especially sodium).
Despite what most government agencies tell you, science has shown that consuming between four to six grams of sodium (that’s eight to 12 grams of salt) is the optimal range, leading to the lowest risk of cardiovascular disease.
So make sure you add enough salt to your meat or consider a delicious electrolyte supplement such as LMNT.
If you aren’t used to eating a lot of protein and fat, your stomach probably isn’t producing enough enzymes and bile juice to properly digest meat, and it might take a while for your digestive system to get used to your “new” diet.
I recommend eating slowly and chewing your food well. That gives your stomach time to release enough enzymes to aid with digestion. You can also take digestive enzymes or diluted apple cider vinegar before meals to support your stomach.
How soon you can expect improvement varies from person to person and depends on the severity of your gut issues. Some people (like me) see improvements within two weeks, but for others it might take a few months. Chances are your IBS developed over several years, so you shouldn’t expect a full recovery within a few days. The best advice I can give you is to be patient and consistent. I promise, it’ll be worth it.
I recommend fats from animal-based sources, including grass-fed butter, ghee or tallow. I also recommend that you avoid vegetable oils, because they’re inflammatory and studies have shown that they can actually cause inflammatory bowel disease (IBD).
The best home remedy to treat and cure IBS is to stop consuming the foods that cause gut issues in the first place. This includes processed foods, but also most plants.
While peppermint oil can feel soothing when you have an upset stomach, it doesn’t work with issues affecting your large intestine. I tried peppermint oil for several weeks while I experienced IBS symptoms and didn’t notice any improvement.
Despite what you might have heard from your dietitian or the media, humans don’t need fiber to maintain a healthy digestive tract and normal bowel habits. I strongly recommend not using fiber supplements (such as Metamucil) or maintaining a high-fiber diet, because both can worsen IBS symptoms.
As far as my experience with fiber supplements is concerned, I can tell you that inulin worsened my symptoms while psyllium husk and acacia fiber had no impact whatsoever on my IBS symptoms.
Wrap-Up: When It Comes to IBS, Managing the Symptoms Doesn’t Fix the Problem
Western medicine has gotten incredibly good at managing the symptoms of ailments caused by our modern lifestyle. Rather than fixing the root causes of modern illnesses, treating symptoms with pharmaceuticals appears to be the default treatment recommendation of many healthcare professionals. I’d argue that’s because selling drugs is more profitable than recommending lifestyle changes.
So instead of advising IBS patients to stop eating foods incompatible with human physiology, most doctors prescribe medication, such as over-the-counter antacids (i.e., proton pump inhibitors), steroids, laxatives, antispasmodics, immunosuppressants, loperamide (Imodium), antibiotics (e.g., rifaximin) and even antidepressants.
But none of these drugs fix the underlying problem. The only way to cure IBS (and similar gut issues) is to adopt a lifestyle that’s compatible with how the human body has evolved over millions of years. That includes the avoidance of foods that cause inflammation and that damage the delicate lining of the gut, better managing stress, and focusing on sleep quality, to name a few.
Check out my article about the core principles of a healthy lifestyle to learn more about these concepts.
If you suffer from IBS and you want to give my tips a try, let me know about your experience in the comment section below!

Michael Kummer is a healthy living enthusiast and CrossFit athlete whose goal is to help people achieve optimal health by bridging the gap between ancestral living and the demands of modern society.
Medical Disclaimer
The information shared on this blog is for educational purposes only, is not a substitute for the advice of medical doctors or registered dieticians (which we are not) and should not be used to prevent, diagnose, or treat any condition. Consult with a physician before starting a fitness regimen, adding supplements to your diet, or making other changes that may affect your medications, treatment plan or overall health. MichaelKummer.com and its owner MK Media Group, LLC are not liable for how you use and implement the information shared here, which is based on the opinions of the authors formed after engaging in personal use and research. We recommend products, services, or programs and are sometimes compensated for doing so as affiliates. Please read our Terms and Conditions for further information, including our privacy policy.

Hi Michael, I am 40 now, and I have been suffering with similar gut symptoms as yours, minus the stomach pain, forever. I am from India, grew up on a pure vegetarian diet plus milk. I had colonoscopies thrice in life, which were both embarrassing and painful with my piles. I had been influenced by the ayurvedic style of eating, which shuns meat and promotes the use of grains and a lot of veggies. I did use this fiber and that ayurvedic medicines all in vain. I believe all these are just natural laxatives.
The first time I found about fiber being the cause of constipation and other gut problems was from a article from constantin. for the last few years, I researched too much and got to know about everything that you have mentioned in your article from your channel and many other supporters of a meat-based diet.
Last month I tried it for the first time, since I have been toying with increasing my meat consumption for the last few years. my breakfast has always been eggs for the last 3 years. I tried to go completely carnivorous. For the first two weeks, I felt that I was completely cured. I had one easy bowel movement in the morning, a few bouts of diarrhea, and had no bloating for the day. sometimes I went once in the evening. I was still taking Vitamin C, which I have been taking for the last few years. I was also eating only two meals.
I am very thin naturally, and in just two weeks, I actually went very thin and had almost no fat on the body, and started feeling I was losing muscles. I researched and I found out I needed more protein and fats. Increasing them perhaps brought back my earlier bloating and my increased time in toilets, like before. I have been drinking coffee too for the taste and to keep me regular in mornings.
I am a bit confused and exasperated to find out that what worked for others didn;t work for me. In the beginning , I took two betaine HCL with my heavier meat diets..but since I have gone too thin and weak and am not able to perhaps digest more meat and fats, so for the last two I have introduced rice into one of my meals, and feeling a little better but not as good as I felt around 10th day of my carnivore.
I also have had many blood tests done around 25 days into this diet and found my fasting insulin high as 44. Still, I feel if I lose more muscle mass, it will perhaps increase the insulin even more than eating rice.
I have written too much, I am sorry for that, but perhaps can you tell what I did wrong and how can I get back to a diet I started believing and get all the said benefits of it, which are eluding me someway.
Hey Ramesh,
Thanks for reaching out! Building and maintaining muscle tissue requires two factors: sufficient protein intake and stimulation (i.e., resistance training). On the other hand, body fat is usually based on surplus calorie intake. Having low body fat isn’t a bad thing. Of course, there is such a thing is having too little body fat but if you can hover around 8-12%, there is nothing to worry.
How much protein can you consume without side effects? Ideally, you want to target about a gram per pound of body weight. Have you combining your protein intake with weight lifting? Without stimulus, your body won’t have any incentive to grow more muscles.
What I’d do is try and figure out what causes your side effects: the extra protein or the extra fat. If it’s the fat and you’re afraid of not getting enough to sustain your energy levels, try including cucumbers, squashes, olives or avocados (depending on what’s available in your region). You could also experiment with seasonal sweet fruits to see which ones you can tolerate.
If you’re low on protein (less than one gram per lb of body weight), see if you can find digestive enzyme supplements (protease) to help with the digestion until your body gets used to it.
Cheers,
Michael
I tried it for 2 weeks and was bound up real bad by doing that.
I had a strangulated hernia that hung outside my body for 3 months before I had to go to the emergency. They pushed it back in. That was more than a year ago. I feel that there is a fold or twist in it and it holds my bowels movement back. Eating a healthy diet kept the stool soft enough to come out. When the stool is formed I have pictures of a cut down the side of the excrement. Indicating to me that something is there with body and allow the excrement to pass but reformed it with that tear, cut or what ever. The gastroenterologist says no , He does not know why. He says it is probably IBS.He does not know the cause of IBS. I had an intuitive look at me and she says it is nerve damage, from what?
Have you ever had a situation explained to you like this before. Now I get relief by using C scorbutic and magnesium situate that I make up. It produces diarrhea. I have a feeling like I have to urinate and I do. I use ProstaGenix. and it works beautifully for my prostate. But then after or during my urination I make a weak attempt to move my bowels. If I do the pain goes out of my prostate area and I have to really try to move my bowels.
I don’t think you want to venture and suggestions but I have to ask.
Hey Harold,
If you believe here might be something physically wrong inside your GI tract, you may want to consider swallowing one of those miniature cameras (capsule endoscopy) that can take photos of your digestive tract. However, the “cut down” you’re describing could be caused by your anus (e.g., hemorrhoids). Have you ever had your rear checked?
It’s needless to say that there is no way to reliably diagnose your conditions over the Internet but chances are, a proper diet (void of triggers) will likely lead to dramatic improvements.
Cheers,
Michael
Hi Michael,
First, I love your products and what you and your family stand for. I read everything that you write about.
I would love for you to write an article about APOE4 and consuming meat and dairy. There’s some information out there, but it’s confusing. My husband and I both follow a carnivore diet. But I have two APOE4 alleles. I’ve heard that I should reduce my saturated fat and eat less red meat and dairy…this of course goes against carnivore. So I just don’t know what to do.
Thanks for any input!
Hey Robin,
You’re one of the lucky ones that make human nutrition even more complex than it already is :)
I have a buddy who has two APOE4 alleles and super high cholesterol and LDL. However, his inflammatory markers are as low as mine. I’m not sure you’ll be able to get a definitive answer on the topic from anyone because there is much we don’t know.
If I were in your shoes, I’d monitor my inflammatory markers (CRP, ESR, IL-6, TNF-a, Lp-PLA2…) and insulin like a hawk. If those markers are low, I would not be too concerned about elevated blood lipids and your risk of metabolic issues or Alzheimer’s. You could also consider replacing some of your saturated fats with monounsaturated fatty acids (e.g., from bone marrow) and even include some wildcaught seafood or high quality pork (pasture raised and heritage).
Finally, you could sign up for revero.com — that’s Dr. Shawn Baker’s medical service that can give you more specific information and guidance.
I hope that helps!
Wow, thank you so much! I wasn’t expecting such an in-depth reply.
I really do appreciate it, and I’ll look into everything that you recommended.
With great gratitude,
Robin
You’re most welcome, Robin!
Hello Michael,
Quick question on all of this – is it possible that this diet may temporarily worsen IBS symptoms before you see improvement? I’ve been on this diet for about two weeks, and the first few days were great, but now my symptoms are becoming far worse than they were even with a standard low-FODMAP diet. I’d like to stick with this diet in the hopes that it eventually brings relief, but I’m finding it very hard to stick with it when it seems my stomach and intestines hate this diet.
All the best,
Alex
Hey Alex,
I’d say that any dietary change can worsen or cause different symptoms temporarily. It’s also possible that you’re not making enough digestive enzymes or have enough stomach fluids and you’re overloading your system. Can you share more information about your symptoms, what exactly you eat, how much and when? That said, maybe dial it back a bit by including some of the least-toxic plants in your diet (peeled and deseeded cucumbers, zucchini or squashes). You can also drink diluted apple cider vinegar before meals to get the juices flowing.
Cheers,
Michael
Hi Michael,
Thanks for your reply! My symptoms are mostly stomach and intestinal discomfort and pain after eating, which usually lasts for a few hours. While I still have irregular bowel movements, the frequency has gotten better since going carnivore (from 2-4 times a day to 1-2 times a day).
I am eating a variety of unprocessed meats, salt and butter, 2-3 meals a day. Originally just meat and salt, but I added butter as I was losing weight and don’t want to. Only drink water. I do take digestive enzymes with most meals, but I’ll try adding ACV as well.
I’ll certainly stick with this diet for a bit longer, I want to at least give it a fair shot before giving up on it!
Thanks,
Alex
Hey Alex,
I’d definitely give it a few weeks to a few months. Whatever damage has been done takes a while to heal. You can also consider adding something like Collagen & Colostrum to the mix to support the healing process.
Cheers,
Michael
Thank you for this article. Love the information you offer.
My husband is struggling with a form of IBD. How much honey per day? And when would be the best time in the day to take it?
He’s been carnivore for the last 3 months. The last 2 was strict red meat, water, broths and electrolytes. He’s went down to one bowel movement per day, but it’s never a solid stool, always pure water. It’s like we can’t seem to improve him more than this. He’s been on Megasporebiotic. Wondering about kefir. I started introduing egg yolks into his meals for added nutrition, we’ll see how that goes. It’s been very challenging to help him hold electrolytes, he’s a little stronger, but he’s stil not able to do most tasks , he’s still weak. He’s only 47 and he’s so frustrated. Do you think his healing process is a normal pace for something like this?
Hi Anita,
honey isn’t necessary for healing. It’s more like a crutch if you feel like you need some carbs. I’d not eat more than 1-2 tablespoons a day but it’s likely nest to avoid it entirely (at first). Electrolytes are fine but keep in mind that consuming too much can lead to loose/watery stools. How much electrolytes is he taking and what kind?
I’d cut out the Megasporebiotic unless you know for certain he handles plant fibers well. Has he ever had a stool analysis to see if he has parasites or certain bacteria that might require extra treatments?
I’d love to try the carnivore diet. I just don’t have the funds to but the high quality meats that I would prefer. Plus, I am not allowed to cook organ meat in the house haha.
Hey Matt,
I firmly believe that consuming conventionally-raised meat (e.g., inexpensive cuts from Costco or Walmart) is better than not eating meat. In fact, both Aldi and Walmart sell grass-fed ground meat for $5-6 a pound. That’s relatively affordable. Regarding the organ meats, check out shop.michaelkummer.com for freeze-dried options and wait for the next sale (Labor Day is coming up)…
I hope that helps!
I’ve never heard anyone else say that inulin (also called chicory root fiber) is a trigger. It causes huge issues for me as does maltodextrin and sulfites.
Yeah, inulin and I are no friends :)
Hello,
First of all, thank you for the information you shared; It is generally difficult to find quality and first-hand information shared. I was diagnosed with SIBO and came across your article in my research because I thought it was similar to IBS. I know from experience when I eat meat I am okay but when I eat salad, I will destroyed by pain :) I am currently working with a dietitian and for the last month, I have been eating only meat and one zucchini/30 grams of lettuce maximum. Despite this, I have very annoying bloating. When I asked my dietitian, she stated that: “zucchini is low FODMAP and it shouldn’t disturb you”. Reading your article made me look at zucchini in a new way; so I thank you. I also have a question: I use olive oil(or have constipation) while cooking and occasionally I drink freshly squeezed, diluted lemon juice; do you think these will have negative effects?
Best regards,
EVOO and lemon juice should be fine but everyone responds differently to certain foods. I never heard anyone responding negatively to EVOO but lemon juice could be irritating if you’re sensitive.
Regarding zucchini, I’d agree with your dieting but make sure you peel and deseed the zucchini before consuming it. The peel and seeds have anti nutrients that could trigger you.
Hi, I’ve been suffering from IBS for about 2 years now. I am 23 years old and from Germany. I’ve been going to doctors and a nutritionist here, but nothing has helped so far. I’ve also been researching studies in Germany, but sadly, people here kind of overlook the problem. So I started to do my research in English. I came across a lot more people who talked about their IBS and what helped them heal their gut. Many of them suggested trying the low FODMAP diet. So I did, but again, there was no real improvement. It was also very confusing because every low FODMAP list is different. Then I came across you and other people like you who were stating that just eating meat would cure IBS. I’m honestly kind of scared to try this out because I suffer from really bad bloating and constipation, so wouldn’t meat make that worse?
I also take supplements like papaya enzymes, probiotics, and magnesium.
Do I have to eat meat for breakfast, lunch, and dinner, or should I just eat one meal a day that contains meat? I would be very grateful for a reply.
Cheers, Liza
Hi Liza, thanks for reaching out! I completely understand your hesitation—it’s natural to feel uncertain when trying something new, especially with ongoing IBS symptoms like bloating and constipation. Many people with IBS find that certain diets, like the low FODMAP diet, can be confusing or inconsistent. That’s one of the reasons why I recommend simplifying things with a more meat-based approach.
When it comes to bloating and constipation, eating only meat can actually help because it eliminates many of the fibers, plant toxins, and fermentable carbohydrates that often irritate the gut and contribute to IBS symptoms. Meat is highly digestible and doesn’t ferment in the gut like fiber-rich plant foods, so it could potentially relieve those issues instead of worsening them.
You don’t have to jump straight into eating meat for every meal if you’re not ready. Some people start by incorporating one or two meals of just meat per day and gradually build up from there. You can try easily digestible meats like beef, lamb, or even chicken to see how your body responds. Over time, you can adjust based on how you feel.
Regarding your supplements, it’s good that you’re supporting digestion with enzymes and magnesium, but sometimes probiotics can irritate IBS in certain individuals. You might want to experiment with reducing or eliminating them temporarily to see if it makes a difference.
I’d say go at your own pace, and if you’re feeling curious, you can test out a few small meat-based meals and see how your body reacts. Everyone is different, so it’s important to listen to your body and take it step by step.
Let me know if you have more questions, and good luck with your journey!
This is not really a cure for IBS but a mitigation strategy. No one has found a cure for an IBS’er to return to a normal diet and live like others do. With something like diabetes, the doctor diagnoses it and everyone helps the diabetic. With IBS, the doctor can find nothing wrong and we are left without support in no man’s land.
There will always be certain foods we can’t eat without paying a big price. Meat will always be the easiest, but if you are a vegetarian, it can be done. Everyone in life is given unique challenges. If I’ve inadvertently eaten the wrong food, I’ve found bromelain to be of some help.
You’re operating under the wrong assumption that humans are supposed to be able to eat whatever and stay healthy. That’s simply not true. Humans have consumed specific foods (and learned how to process them to reduce their relative toxicity) for millions of years. Most of the foods (or food-like substances) we consume today bear no resemblance to the foods our physiology is adapted for. Curing IBS means consuming foods we’re made to consume and avoiding those we’re not capable of. Your definition of a “normal” diet is likely anything but normal as far as our physiological capabilities are concerned.
Your information makes perfect sense. I have suffered with IBS-D for many years and find that it’s worse during times of stress. I’ve tried so many things to no avail so I’m going to try your diet strategy. What I are your typical meal plans? Do you eat 3 times a day or several small meals? I just need some guidance please. Thank you for sharing your story. And best wishes to you and your family.
Hey Netia,
I usually eat two meals a day, including eggs and meat in the morning and more meat in the afternoon. Since I no longer have IBS, I get to eat more than just meat. In other words, I follow an animal-based diet – see https://michaelkummer.com/animal-based-diet/
Michael, I’m 77 and was diagnosed with IBS this past fall. My background of the way I have eaten was like you, started out paleo in 2017 because I needed to lose wait and get my sparkle back. I went Keto about six months later. In 2020 I was ketovore..mostly ‘vore. the beginning of 2021 I ended up getting COVID which took away my taste. I was living on protein drinks because I couldn’t bring myself to cook. I had my son bring me Pakistani food because I thought I would be able to taste the wonderful spices. That set me back to the old way of eating. I had some set backs in 2022 and 2023 emotionally and ended up with depression and spiraled down to my current IBS . Being I was almost carnivore for two years and ended up eating the traditional American way of eating, could that have triggered the IBS along with the stress of my life?
I’d say that’s very likely. Stress plays a big role in gut health and when combined with less-than-ideal food, you have a recipe for disaster.
I have lost weight over the couple of months. Would carnivore-based diet helps me to gain weight as well? Thanks
Eating ample of amounts of animal-based protein combined with resistance (weight) training is the best way to gain lean muscle mass. I assume that’s what you mean by “gain weight.”
Hi,
Can I eat gummy bears and bread with chocolate cream on it? Will it heal my guts? Also can I eat ice creams from time to time, like everyday? And chips? Will it cure my gut?
I just assume that your questions are sincere and you don’t know any better instead of deleting the comment. No you cannot eat any of that if you want your gut to heal.
Hi there,
I wish I read your article few years ago.
About honey, it’s high in fructose and may worsen digestive issues among some people with IBS (like me).
Also, you say you cured your IBS. Hmm… you didn’t. You just eat the right food, meat 😉 and if you started eating as you did in the past, the symptoms would come back.
Thanks for sharing!
Hi Katerina,
honey doesn’t work for everyone but I have yet to come across anyone who meat + honey has caused issues. Obviously, gut issues will return if you resume consuming foods that aren’t compatible with human physiology. The same could be said about resuming smoking cigarettes after overcoming lung cancer.
Gday Michael. I’m on day 71 carnivore. Fairly strict.Lost 6 kg in the first 6 weeks mainly off my gut. Suffered all my life with diarrhoea & I’m happy to say that’s all gone. Minimum 2 minute cold shower every morning. I’m just about to hit 75 and am feeling great. Never been on any medically drugs. Don’t even have a doctor. Cheers. David.
Thanks for sharing your feedback, David! Way to go!
Is rice ok to eat? My diet consists mostly of 2 English muffins in the morning along with a banana, then at night a dinner of chicken or fish with rice and a very small portion of carrots. Sometimes a baked potato instead of rice. I use olive oil on most things. Zero dairy.
So I find myself wondering if, according to your plan, white rice is ok to have with dinner. I have had horrible IBS all my life and I’m 66 now. Thanks!
Hey Brian,
neither rice nor muffins, bananas or carrots are ideal if you’re trying to heal from IBS. I thought the article made it relatively clear what you should and shouldn’t eat :)
Cheers,
Michael
I made it a mission to get my gut issues under control and it’s taken me 3 years because I started with low fodmap and then elimination diet which took 6 months. I did everything like GF, supplements, etc one at a time to see which gave results. I now have no issues unless I’m having an overly stressful week or something. I eat very low carb, low sugar, make sure to keep my vitamin levels good (I’ve researched each individual supplement to make sure I’m getting the best form) and never forget my magnesium because that made a huge improvement. All that to say that I agree with everything In your article and all of those suggestions helped me tremendously in my journey and some are permanently in my routine. For example I don’t take probiotics anymore, I just eat kimchi or real sauerkraut a couple times a week, but the probiotics were a must for awhile. Especially since I had bacterial meningitis and was on the strongest antibiotics for weeks in the hospital which definitely worsened my ibs and I needed to replace all the good bacteria. So for anyone suffering from ibs (mine was severe C), if you follow the advice in the article while also doing your own research to see what else you need to do or not do since everyone’s ibs can be a little different, eliminate inflammatory foods for awhile like gluten, walk every day if you can’t exercise so that you keep everything moving correctly, you WILL get better! This article is saving you many hours of research (I know because I’ve done the many hours unfortunately lol) so just start here!
Thanks so much for sharing your (success) story, I really appreciate it!
Thank You Michael! Just wanted to say the the Simply 03 is said (by FDA) that it does not support gut issues or kill parasites. It appears to be just anti-inflammatory.
My best to you and yours!
Bernadette Fritz
That FDA warning is meant as a joke because the FDA prevents supplements manufacturers from making any health claims. So the owner of SimplyO3 decided to be sarcastic on the labels. In other words, ozone does work for gut issues and parasites!
Sir,
I am from India and suffering from IBS since last 5 and half years. Wasted tonnes of money on doctors and medicine, probiotics, antibiotics etc etc , but didn’t get any result. With time the symptoms are getting worse and I am not able to manage it. Meat based diet is not possible for me because I am vegetarian. Stress level is very high and sometimes suicidal thoughts comes to mind but seeing the family I try to live …but it’s getting worse day by day…. I am preparing for exams but half the time I am frustrated with this gut issue.Please suggest something
Thanks
Hi Ankita,
If you want to be healthy (mentally and physically), you have to feed your body in a way that’s appropriate for human physiology and consistent with evolution. Vegan or vegetarian diets are NOT appropriate for humans not are they consistent with human evolution.
Ultimately, you have to decide if the convictions and believes that made you follow a plant-based diet are more important than your health. If you start replacing plants with meat, I’m convinced both your mental and physical health will improve dramatically. In the meantime, please consult a professional to talk about your suicidal thoughts. All the best my friend.
Cheers,
Michael
Hi Ankita,
Half of the population must be facing this ibs issue. So don’t lose hope. Try changing food pattern or consult doctor. Even you can try ayurveda medicine, no side effects will be there.
I was suffering from IBS since a long time, I switched to fatty protein (Keto diet) diet 5-6 months ago and have not observed any signs of IBS ever since. Since I belong from a part of India where it’s hard to obtain beef and pork on a daily basis, so my diet mainly consists of chicken and fish.
My friend who also suffers from IBS since a long time recently got her blood work done and has found many vitamin deficiencies. Her diet has been all vegetarian throughout her life. I have asked her to introduce dairy products and eggs in her diet to get some protein and vitamins. She is also lactose intolerant. I also asked her to discontinue all types of cereals and grains from her diet. I have planned on eliminating legumes and pulses in a month, because sudden exclusion could dishearten her from continuing in this path. Being a vegetarian all her life it gets really difficult for her to not consume grains, do you have any further suggestions with regards to helping her transition smoothly?
Small improvements are the way to go until she gets comfortable with those dietary changes. I’d definitely remove whole grains first and stick with processed grains (e.g., white rice). I’d also incorporate organ meats (offal) into her diet to make sure she gets all the nutrients her body needs. If fresh organs isn’t an option, consider freeze-dried capsules, such as the ones we sell at MK Supplements (shop.michaelkummer.com). I know beef isn’t a great choice for your region, so you might have to try and get fresh goat organs.
Hi Amartya, I am from India too and suffering from IBS. Could you please help me with the diet that you have followed.
Hi Michael,
My husband is suffering from ulcerative colitis.
Can you please share diet plan for a week with me and also tell me what all spices can I include in his diet.
Usually in how much time should we start seeing the results. ( so that we are ready mentally, understand it varies person to person). Please help.
The diet plan is pretty simple: Meat (ideally from ruminant animals), animal fats (e.g., tallow, butter or ghee), salt and water. No spices besides salt. I’d give it 30-90 days.