Acute inflammation is a crucial mechanism that helps the body heal damaged tissue (e.g., after an injury) and fight infections that enter the bloodstream. But if the body stays in an inflammatory state for an extended period, that chronic inflammation can trigger the development or progression of diseases including Alzheimer’s, rheumatoid arthritis, heart disease, cancer, diabetes and many others.
The CDC broadly defines chronic diseases as illnesses that last more than one year. In contrast to infectious diseases, the cause of chronic diseases is usually not viral infections, microbes or other environmental pathogens. Instead, chronic health conditions often develop as we age.
What most people don’t know is that chronic inflammation (and thus, chronic disease) is largely driven by lifestyle factors, such as diet, environmental toxins, exercise and sleep.
In this article, I’ll explore the inextricable link between inflammation and chronic disease and highlight the lifestyle changes you can make to significantly reduce your risk of developing a chronic disease as you age.
I’ll also talk about what foods can cause chronic inflammation, and why lowering inflammation with anti-inflammatory foods or medication is often counter-productive.
Before we get into the nitty-gritty, let’s go into more detail about the difference between acute and chronic inflammation and briefly talk about what happens in your body when the immune system responds to injuries or foreign invaders with inflammation.
Acute vs. Chronic Inflammation

When we think about inflammation, we usually envision swelling, redness, and sometimes pain or itching. On a molecular level, the body’s inflammatory processes is controlled by your immune system, and it involves signaling pathways and substances, receptors, inflammatory cells, and target tissue.
Here’s how it works: When tissue in your body is injured by bacteria, trauma, toxins, irritants, heat or other causes, the immune system responds by signaling to the damaged cells to release chemicals such as histamine, bradykinin and prostaglandins. These substances in turn act as a signal to the neighboring cells to increase blood flow and the permeability of the blood vessels, and to leak white blood cells into the affected tissue. This process results in swelling.
What’s important to understand is that acute inflammation — which happens, for example, when you get stung by a bee and your hand swells — is a crucial process because it helps the body heal the damaged tissue. In the case of a bee sting, the immune system backs off and the inflammation subsides once the bee venom has dissipated.
Problems arise when the root cause of inflammation persists, like if you were to get a splinter in your finger and fail to remove it. In such a case, the immune system keeps releasing inflammatory substances for as long as the foreign invader (the splinter) remains in your finger.
When the immune system stays activated for a long period of time, we call that chronic inflammation, and it causes progressive damage to the affected tissue.
Inflammation and Chronic Disease: An Inextricable Link
There are many types of foreign invaders that cause the immune system to spring into action, including environmental toxins and inflammatory compounds in food.
For example, the consumption of linoleic acid — one of the omega-6 polyunsaturated fatty acids found in high concentrations in vegetable oils, nuts and seeds — can trigger an inflammatory response, especially in people who carry a variant of the FADS1 gene.
When you get stung by a bee and your hand swells, you notice it instantly. But when inflammation happens inside your body, it’s not as immediately apparent. In fact, you may not even realize you’re having an inflammatory response. But over time, this internal inflammation can degrade your health and lead to the development of chronic diseases.
For example, inflammation contributes to the aging of the brain in a process that scientists call “inflammaging,” and it may be one of the factors behind several age-related illnesses, including Alzheimer’s, macular degeneration, atherosclerosis, amyotrophic lateral sclerosis and others.
Inflammation contributes to the development of chronic pulmonary diseases, is the leading cause of asthma, and is an aggravating factor in rheumatic diseases like arthritis. It’s also linked to an increased risk for chronic kidney disease, cardiovascular disease, and several gastrointestinal problems (such as Crohn’s disease and ulcerative colitis). Inflammation is even related to metabolic syndrome, insulin resistance, diabetes mellitus and cancer.
To better explain how inflammation influences the development of chronic diseases, let’s take a look at two widespread health problems that affect millions of people every year: cancer and diabetes.
Inflammation and Cancer
Scientists have discovered that even low-grade inflammation plays a role in the development and progression of cancer.
Cancer feeds off inflammation, so to speak, because inflammatory mediators increase the blood flow to affected areas. In turn, this increased blood flow delivers nutrients to cancer cells. As a result, chronic inflammation may be one of the risk factors associated with prostate cancer, breast cancer, gastric cancer, and other manifestations of the disease.
Some inflammatory mediators are therapeutic when the body releases them in normal concentrations, but they start to create health problems when they’re unregulated.
For example, there’s a molecule called tumor necrosis factor alpha (TNF-α) that has anticancer potential when secreted by white blood cells as part of the immune response system. However, it feeds cancer and fuels many other health issues when cancer cells release it disproportionately.
Inflammation and Diabetes

The link between inflammation and diabetes is a bit more complicated than the link between inflammation and cancer.
When you consume carbohydrates, your liver converts them to glucose. Your cells use that glucose for fuel, with the help of a powerful hormone called insulin and a substance called the insulin receptor substrate 1 (IRS-1).
If you consume more carbohydrates than needed to fuel your cells, insulin helps store the excess glucose as fat so that it can be used for energy in the future.
The ability to turn glucose into fat has been an important survival mechanism throughout evolution because it enables humans to go without food for long periods without starving. The problem is that in modern society, chronic overconsumption of highly-processed carbohydrates creates a significant energy surplus.
That energy surplus in turn causes fat cells to:
- Become resistant to insulin, prompting the pancreas to pump out even more of this powerful fat-storage hormone.
- Grow in size, which leads to the release of cytokines and other inflammatory substances.
Once you’ve reached a point where the insulin your pancreas produces isn’t enough to keep your blood glucose levels in check, you have Type 2 diabetes.
Additionally, those inflammatory cytokines create systemic inflammation that can cause alterations in the pancreatic tissue and blood vessels (as well as elsewhere in the body), leading to an increased risk of developing Type 1 diabetes.
Plus, inflammatory cytokines from excess fatty tissue and pro-inflammatory foods trigger a molecule called suppressor of cytokine signaling 3 (SOCS-3). This molecule interferes with IRS-1, causes insulin resistance, and speeds up the progression towards diabetes.
The Link Between Your Gut, Inflammation and Chronic Disease

One organ that appears to play a pivotal role in the progression of inflammation and chronic disease is the gut.
As you probably know, one of the many roles of our digestive system is to break down the food we eat into amino acids (the building blocks of proteins) and fatty acids (the building blocks of fat) that our body can then use for a variety of functions, including the creation of vitamins and the building of muscle tissue.
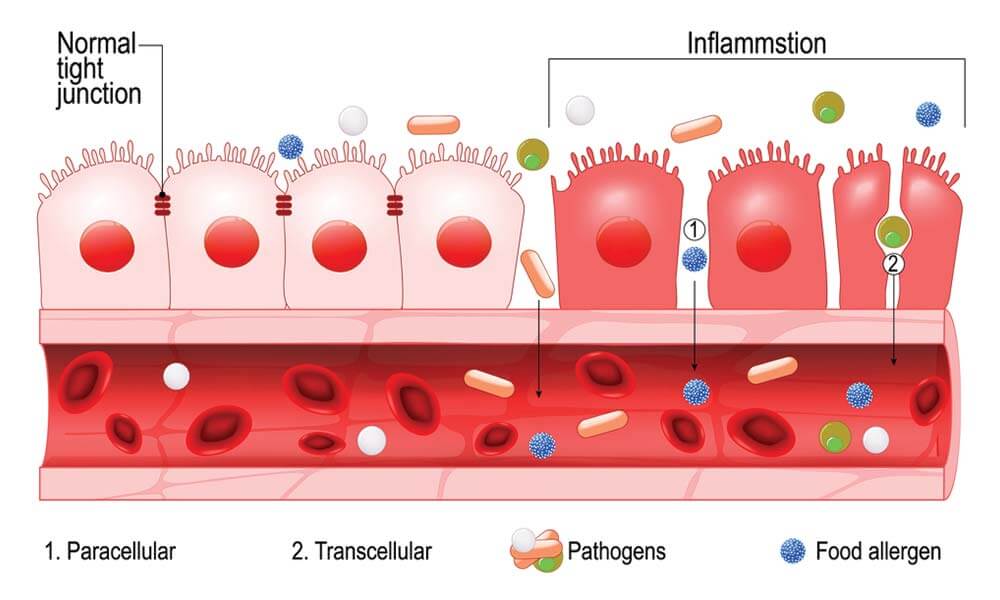
You might also know that the gut has a thin lining (only a few cells thick) that prevents undigested food components from entering the blood stream.
However, certain lifestyle factors — including a poor diet, stress, alcohol consumption and cigarette smoking — can damage that thin lining, leading to what’s known as a leaky (or permeable) gut.
A leaky gut allows undigested proteins (and other toxins) to enter the blood stream, where they’re identified as foreign invaders by the immune system.
As a result, the immune system responds with inflammation in an attempt to neutralize those invaders. If you don’t fix your leaky gut by making the appropriate lifestyle changes, your immune system will remain active, thus leading to chronic inflammation that can ultimately cause the development or progression of chronic diseases.
Symptoms of Chronic Inflammatory Conditions

Considering that inflammation is at the root of most chronic diseases, it’s safe to assume that if you have any of the medical conditions listed below, you also suffer from chronic inflammation.
- Any autoimmune disorder, including Addison’s disease, autoimmune vasculitis, celiac disease, Graves’ disease, Hashimoto’s thyroiditis, inflammatory bowel disease (IBD, including Crohn’s disease and ulcerative colitis), Myasthenia graves, multiple sclerosis, pernicious anemia, psoriasis, rheumatoid arthritis, Sjögren’s syndrome and Type 1 diabetes.
- Alzheimer’s (which is increasingly referred to as Type 3 diabetes).
- Cancer.
- Cardiovascular disease.
- Chronic fatigue syndrome.
- Dementia.
- Irritable bowel syndrome (IBS).
- Metabolic syndrome.
- Pre-diabetes.
- Stroke.
- Skin rashes or eczema.
- Type 2 diabetes.
But even if you haven’t been diagnosed with any of those conditions, you may experience any (or a combination) of the following symptoms that are often caused by chronic inflammation:
- (Chronic) fatigue.
- Achy muscles (not caused by strenuous exercise).
- Swelling and redness (not caused by acute inflammation).
- Low-grade fever.
- Trouble concentrating (not caused by an obvious reason, such as poor sleep).
- Numbness and tingling in the hands and feet.
- Hair loss (not caused by sudden dietary changes or nutrient deficiencies).
- Skin rashes (not caused by insect bites, poison ivy or similar).
- Extreme thirst.
- Rapid weight loss.
- Belly pain, bloating and diarrhea.
If you frequently suffer from any of these symptoms, I recommend consulting a knowledgeable health professional and getting a blood test to look for certain biomarkers that might indicate a metabolic issue.
Specifically, C-reactive protein (CRP), plasma viscosity (PV) and erythrocyte sedimentation rate (ESR) are inflammatory markers you can test for. Unfortunately, none of those biomarkers will tell you what’s causing the inflammation. But at least you’ll know if there is chronic inflammation inside your body.
Top 5 Causes of Chronic Inflammation
Now that you understand the relationship between inflammation and chronic illnesses, let’s take a look at some of the ways your lifestyle choices affect your health and influence inflammation.
From there, we can better understand how to develop prevention strategies that will lower your risk for chronic ailments or slow their development and progression.
The best course of action to stop chronic inflammation is to address the factors that are causing it. The most common causes of inflammation (in alphabetical order) include:
- Alcohol consumption.
- Chronic stress.
- Cigarette smoking.
- Dietary factors.
- Environmental toxins.
Let’s dive into each of these factors in order to better understand what you should and shouldn’t do to reduce inflammation.
1. Excessive Alcohol Consumption
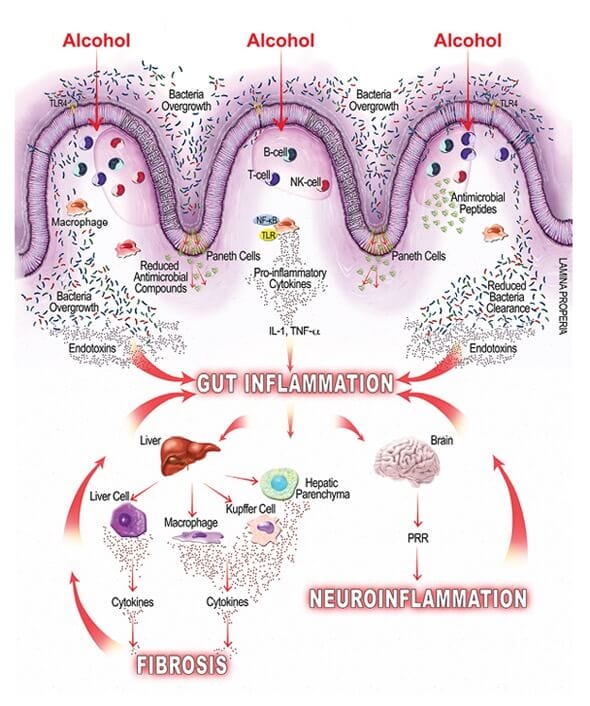
Alcohol can impact the body’s inflammatory response in several ways. For example, chronic alcohol consumption damages the lining inside the gut, increasing the risk of leaky gut.
Excessive alcohol consumption can also increase the body’s transfer of the gut microflora-derived lipopolysaccharide (LPS) — an inflammatory compound that is thought to be derived from a breakdown in the intestinal wall and that can lead to the development and progression of alcoholic liver disease.
Additionally, alcohol impairs the interaction between the gut, liver and brain (and several other organs) that are responsible for balancing the body’s inflammatory response.
In summary, excessive alcohol consumption leads to chronic inflammation and a range of associated medical conditions. If you’re experiencing symptoms of chronic inflammation, I highly recommend that you stop drinking alcohol or that you significantly reduce your intake.
2. Chronic Stress

Studies have shown that chronic stress triggers the release of inflammatory cytokines and disrupts the balance of pro and anti-inflammatory chemicals in the body.
What’s interesting is that there appears to be a connection between the neuroendocrine system (responsible for the release of stress hormones, such as cortisol) and the immune system.
In other words, stress can trigger an immune response. So if you’re under chronic stress, there is a good chance that your immune system is overly active as well, increasing the likelihood of chronic inflammation.
As a result, your state of mind can have a direct impact on your physical health. If you’re struggling with chronic stress (like most of us are to varying degrees), I highly recommend incorporating stress mitigation techniques into your regular routine, including breathing exercises, meditation and cold plunging.
There are also a number of effective stress relief devices that you can leverage.
3. Cigarette Smoking

Despite the tobacco industry’s 35-year-long denial that smoking causes lung cancer, it’s well established that smoking is harmful to your health.
One of the many ways the toxins in cigarettes cause chronic inflammation is by activating certain white blood cells (i.e., neutrophils) which in turn “release molecules that increase inflammation,” ultimately causing damage to various tissue in your body (including your lungs) and cancer.
So if you’re a smoker, it’s safe to assume you’re suffering from chronic inflammation that significantly increases your risk of developing cancer or other chronic diseases.
4. Dietary Factors

Modern diets play a major role in the development and progression of chronic inflammation and disease.
Humans have evolved over millions of years on a diet centered around animals (meat, organs and fat) and the least-toxic seasonal plants. But most of the foods — or shall I say, the “food-like substances” — available at the grocery store today didn’t exist until a few decades ago.
I’m referring to things like:
- Artificial colors and sweeteners.
- Fake meat.
- Certain fried foods.
- Industrial seed oils (also known as vegetable oils).
- Refined carbohydrates (white bread, flour, etc.).
- Sugary beverages.
All of these substances have the potential to trigger an inflammatory response that, over the course of a few decades (or less, in some cases), can lead to the development of chronic disease.
As a result, I highly recommend avoiding these substances as much as possible. Instead, stick to the foods our ancestors and early humans consumed for millennia, like pasture-raised meat (ideally from ruminant animals), wild-caught seafood, raw dairy (unless you’re sensitive to it), raw honey and the least-toxic seasonal plants.
You can learn more about the foods you should and shouldn’t eat in my healthy lifestyle guide. I also recommend checking out my article comparing meat with plants to learn more about why I recommend avoiding most plant foods.
5. Environmental Toxins

You’re probably aware that certain environmental toxins, such as mold and heavy metals, can lead to chronic inflammation and health issues.
However, you may not have known that most plastic food storage containers, as well as tap water and personal care products, are also full of pro-inflammatory toxins that can severely impact your health and well-being.
My recommendation is to avoid all plastic food storage containers, to filter your drinking water (we use a whole-house purification system), and to look for toxin-free personal care products.
To learn more about why, check out my blog post detailing how xenoestrogens make you infertile and sick and watch my YouTube video that lists the non-toxic household products we use in our home.
Myths and Misconceptions
There are a lot of misconceptions about the issue of reducing inflammation. Even in the realm of acute inflammation, most people — including many healthcare professionals — apply the wrong treatment methods.
Case in point: most people think that applying ice to a sprained ankle is the best course of treatment, because the ice reduces inflammation. But the truth is that reducing acute inflammation is often counter-productive since it impairs the natural healing process that relies on the body’s ability to deliver sufficient oxygenated blood flow to the injured tissue.
So if you suffer from a sports injury, chronic knee pain or even arthritis, ice is the wrong way to go. Instead, you want to increase blood flow to the affected area using methods such as photobiomodulation (laser-based red light therapy).
The traditional methods for treating chronic inflammatory disorders are often equally misguided and involve non-steroidal anti-inflammatory drugs (NSAIDs), steroid injections, or even natural remedies such as turmeric, ginger or garlic.
However, masking parts of the body’s inflammatory response (such as its pain signals) is ineffective and can exacerbate the problem, especially if you don’t concurrently address the root cause of the inflammation.
For example, NSAIDs have been shown to degrade healthy tissue, slow down recovery and even foster chronic inflammation.
Remember, inflammation is your body’s way of telling you that something is wrong. Suppressing that cue doesn’t fix the underlying issue.
As a result, I don’t recommend leveraging anti-inflammatory compounds — natural or otherwise — to treat chronic inflammation. Instead, remove the underlying root cause. If you’ve ruled out everything else (nicotine, alcohol, stress, etc.), the culprit is likely your diet.
Frequently Asked Questions
Rheumatoid arthritis is an autoimmune condition that causes the deterioration of cartilage and bone tissue in the joints.
Autoimmunity occurs when an overactive immune system starts attacking healthy cells as part of an inflammatory response.
For many years, scientists believed that in the case of autoimmune conditions such as rheumatoid arthritis, the immune system simply malfunctions by engaging without the presence of foreign invaders.
However, today we know that the immune system might be (over)reacting to environmental toxins and certain compounds in the food we eat.
Specifically, nutrition plays a critical role in the development of a leaky gut that, if left untreated, causes systematic inflammation that can lead to autoimmune issues, including rheumatoid arthritis.
Based on what we know from human evolution and by observing modern hunter-gatherer tribes (e.g., the Hadza), the best diet for optimal health is centered around pasture-raised ruminants, raw honey, raw dairy and the least-toxic plants.
While such a diet may include some plants — especially sweet fruits — that have anti-inflammatory properties and antioxidants, you don’t need to go out of your way to consume them.
For example, resveratrol is an antioxidant and anti-inflammatory molecule found in grapes and other fruits with polyphenols. We know that it reduces the formation of free radicals, the concentration of TNFα in the blood, and the expression of several inflammatory mediators.
However, just because resveratrol appears to reduce inflammation in isolated tests, that doesn’t mean it’s beneficial to your health. A randomized placebo-controlled clinical trial with resveratrol revealed no beneficial effects on the metabolic syndrome.
If you follow a species-appropriate diet for humans, exercise regularly, get enough sleep and manage stress well, you’ll likely get all of the nutrients you need to stay healthy from the food you eat.
However, life isn’t always easy and food isn’t as nutrient-dense as it used to be, thanks to deteriorating soil quality and other factors. As a result, I believe that certain whole-food supplements are a great way to bridge any nutritional gaps and to help the body better deal with daily stressors.
My go-to supplements are freeze-dried organ meats (in particular, freeze-dried liver capsules) and Magnesium Breakthrough before bedtime. I don’t take or recommend plant-based extracts such as resveratrol or curcumin for the reasons I outlined above.
I also avoid omega-3 supplements because there is no easy way to make sure they’re not rancid. Instead, I consume suet and tallow from grass-fed cows as well as wild-caught salmon and sardines — all of which are excellent sources of omega-3.
Epidemiological studies have correlated the Mediterranean diet with lower levels of inflammation. As a result, I’m comfortable saying that the Mediterranean diet is healthier than the standard American diet (SAD).
However, I’m a proponent of consuming foods that mimic what humans have eaten over millions of years as part of evolution. That type of ancestral diet doesn’t include many of the foods that are part of the Mediterranean diet, such as whole grains, legumes and most vegetables.
Final Thoughts on the Link Between Chronic Disease and Inflammation
As the evidence I linked to throughout this article shows, there is an undeniable connection between our dietary choices and inflammatory pathways, as well as between inflammation and chronic disease.
Looking at statistics from the CDC, we can see that the rate of chronic illnesses has increased dramatically over the past few decades. At the same time, our food choices have deteriorated, and the food we eat has little in common with what our ancestors used to eat — the meat, fat and organs of animals, pasture raised eggs, raw honey and a few types of seasonal plants.
So it’s no stretch to imagine that the adoption of the Western diet by an increasingly large portion of the world’s population (especially by adults in developed countries), coupled with a general lack of physical activity and exercise, has had a massive impact on our overall health and well-being. Reversing this trend is an important aspect of chronic disease control.
The good news is that it’s not too late to adopt strategies that will reduce our risk and promote better health outcomes. There are plenty of healthier options available in our modern world. Factors like staying physically active and making educated decisions about the food you consume will reduce the risk of obesity, contribute to disease prevention, and help you achieve long-lasting benefits for your health and overall quality of life.

Michael is a healthy living enthusiast and CrossFit athlete whose goal is to help people achieve optimal health by bridging the gap between ancestral living and the demands of modern society.
Medical Disclaimer
The information shared on this blog is for educational purposes only, is not a substitute for the advice of medical doctors or registered dieticians (which we are not) and should not be used to prevent, diagnose, or treat any condition. Consult with a physician before starting a fitness regimen, adding supplements to your diet, or making other changes that may affect your medications, treatment plan or overall health. MichaelKummer.com and its owner MK Media Group, LLC are not liable for how you use and implement the information shared here, which is based on the opinions of the authors formed after engaging in personal use and research. We recommend products, services, or programs and are sometimes compensated for doing so as affiliates. Please read our Terms and Conditions for further information, including our privacy policy.


What do you think about turmeric to support a healthy inflammation response?
The health benefits of Turmeric is on my editorial roadmap,but I haven’t done enough research yet to give you an immediate answer, so stay tuned :)